Inspire Therapy Candidacy: Qualification Checklist for Sleep Apnea Patients
Introduction — Why Candidacy Matters for Inspire Therapy
The common problem: “CPAP works… but I can’t use it”
CPAP remains the standard treatment for obstructive sleep apnea (OSA). Yet many people struggle in real life—mask discomfort, leaks, dryness, claustrophobia, pressure intolerance, or simply not being able to sleep with the equipment on. If you’ve ever thought, “I know it helps, but I’m not actually sleeping with it,” you’re not alone. A great treatment only helps if you can use it consistently, which is where Inspire therapy may enter the conversation—but candidacy is specific, and not everyone qualifies.
What this guide covers
Below is a patient-friendly qualification checklist (the “Am I eligible?” basics), plus what typically happens during an evaluation so you’ll know what to expect and why some people are approved while others are denied.
Who this is for
This is mainly for adults with moderate to severe obstructive sleep apnea who have trouble using CPAP consistently. Inspire publishes qualification requirements and updates them over time, so eligibility is always confirmed by a clinical evaluation and testing—not by a quick online quiz.
Source: https://www.inspiresleep.com/en-us/qualification-requirements/
— In short, this guide explains who may qualify for Inspire, how candidacy is checked, and what to do next. —
Quick Refresher — What Is Inspire Therapy?
Inspire = implantable hypoglossal nerve stimulation (HNS) for OSA
Inspire is an implant-based treatment for obstructive sleep apnea that uses hypoglossal nerve stimulation—a gentle, timed signal to the nerve that helps control tongue movement.
For a deeper overview, see: https://sleepandsinuscenters.com/blog/inspire-hypoglossal-nerve-stimulation-a-101-guide-to-sleep-apnea-treatment
How it works during sleep (plain-English)
In many people with OSA, the airway narrows or collapses during sleep. Inspire is designed to help keep the airway open by prompting certain tongue muscles to move in a way that reduces blockage while you sleep. Think of OSA like a “soft, flexible tube” that can kink when you relax into sleep; Inspire supports the airway at the right moment—timed with your breathing—so collapse is less likely.
What Inspire is not
- It is not a mask or CPAP device
- It is not intended as a “snoring-only” fix
- It is not for people whose sleep apnea is primarily central rather than obstructive
Professional indications/contraindications: https://professionals.inspiresleep.com/en-us/indications-and-contraindications/
— Bottom line: Inspire is a mask-free, implant-based option for obstructive—not central—sleep apnea. —
Sleep Apnea Symptoms & Why Treatment Is Important
Common symptoms of obstructive sleep apnea
People often seek help because of:
- Loud, persistent snoring
- Pauses in breathing witnessed by a bed partner
- Choking or gasping at night
- Morning headaches or dry mouth
- Daytime sleepiness, brain fog, reduced focus
- Mood changes or irritability
Why untreated OSA can be risky
OSA is more than “just snoring.” Ongoing sleep disruption and oxygen drops can affect quality of life and are linked with concerns involving blood pressure, heart health, and daytime safety (including drowsy driving).
When to seek an evaluation
If symptoms are frequent—or a partner is noticing breathing pauses—it’s reasonable to consider a sleep evaluation. A sleep study helps determine whether OSA is present and how severe it is.
— Key takeaway: If symptoms are frequent, a sleep study clarifies severity and guides next steps. —
What Causes Obstructive Sleep Apnea (OSA)? (And Why It Impacts Inspire Eligibility)
Airway collapse patterns (tongue base vs soft palate vs multiple levels)
OSA doesn’t look the same in everyone. Some people obstruct mainly at the tongue base, others at the soft palate, and many at multiple levels. Inspire candidacy depends heavily on how the airway collapses.
Weight/BMI and airway anatomy
Body weight can influence airway anatomy and collapse. This is one reason BMI often appears in Inspire candidacy discussions—both for expected outcomes and for insurance coverage rules.
Nasal obstruction and other contributors
Nasal congestion, a deviated septum, or chronic allergies may not be the root cause of OSA—but they can make CPAP harder to tolerate and can affect sleep quality. Many patients describe a loop: they want to use CPAP, but they can’t breathe comfortably through their nose with the mask on.
— In short, Inspire works best when your collapse pattern fits its mechanism—and BMI and nasal factors can also matter. —

Inspire Therapy Candidacy — The Core Qualification Checklist (Adults)
Below is a streamlined checklist that reflects common requirements used in real-world Inspire evaluations. Final eligibility depends on your testing results, airway anatomy, and medical history.
Sources: https://www.inspiresleep.com/en-us/qualification-requirements/ and https://professionals.inspiresleep.com/en-us/indications-and-contraindications/
Printable-style checklist (quick scan)
You may be closer to qualifying if you can check most of these boxes:
- Adult (typically 18+)
- Sleep study confirms moderate to severe obstructive sleep apnea
- Sleep study does not show primarily central sleep apnea (central and mixed events are usually required to be a minority of your total events)
- Documented CPAP failure or CPAP intolerance
- BMI is within plan/coverage requirements (varies by insurer)
- Airway anatomy is compatible based on DISE (drug-induced sleep endoscopy)
1) Age requirement
Most adult criteria are written for patients 18 and older.
A separate pediatric indication exists for certain teens with Down syndrome (covered below).
2) Confirmed diagnosis: moderate to severe obstructive sleep apnea
You’ll generally need a sleep study showing moderate to severe OSA—and it must be obstructive in nature. If you’re unsure how to interpret your sleep study, start here:
AHI explained: https://sleepandsinuscenters.com/blog/ahi-score-explained-understanding-your-sleep-apnea-severity
Practical note: Moderate-to-severe OSA typically means an AHI of 15 or greater; exact thresholds and payer policies can vary.

3) CPAP failure or CPAP intolerance (more than “I don’t like it”)
In practice, “CPAP intolerance” means there’s a real barrier to using CPAP enough to benefit from it—often supported by objective compliance data. A commonly used definition is not being able to use CPAP ≥4 hours per night on >5 nights per week, or being unable/unwilling to use it despite genuine attempts and troubleshooting.
Source: https://professionals.inspiresleep.com/en-us/indications-and-contraindications/
Examples of CPAP issues that are often documented
- Persistent mask leak despite refitting
- Claustrophobia or inability to fall asleep with the mask
- Pressure intolerance or frequent awakenings
- Aerophagia (air swallowing/bloating)
- Nasal blockage, dryness, or skin irritation that limits use
Important reminder: Patients should not self-diagnose CPAP intolerance without clinical guidance; documentation and clinician input are typically required for candidacy and insurance review.

4) Body Mass Index (BMI) requirements (clinical vs insurance rules)
BMI is one of the biggest “it depends” areas. Clinically, programs may evaluate candidates across a range of BMIs (some up to 40), but many insurers use stricter cutoffs (often low-to-mid 30s), which vary by plan and region.
Sources: https://professionals.inspiresleep.com/en-us/indications-and-contraindications/ and https://www.brighamandwomensfaulkner.org/programs-and-services/sleep-medicine-and-endocrinology/sleep-medicine-inspire
Why BMI can affect outcomes and approval
BMI can correlate with airway collapse patterns and response rates. Separately, coverage policies may set BMI thresholds for approval.
If your BMI is above your insurer’s cutoff
“Not right now” doesn’t always mean “never.” Many patients discuss safe, medically supervised weight management with their clinician and recheck eligibility later. Your care team can help set realistic goals and timelines tailored to you.

5) Anatomical eligibility (a common deciding factor)
Even with the right AHI and CPAP history, anatomy matters. Most evaluations include an airway assessment to confirm your collapse pattern matches what Inspire is designed to treat.
Drug-Induced Sleep Endoscopy (DISE): what it is and why it matters
DISE is a procedure done under sedation so your clinician can observe your airway in a sleep-like state. It helps answer the key question: where and how does the airway collapse?
Key “rule-out” finding: complete concentric collapse at the soft palate
A commonly cited contraindication is complete concentric collapse at the soft palate on DISE—this pattern is considered incompatible with standard Inspire therapy criteria.
Source: https://professionals.inspiresleep.com/en-us/indications-and-contraindications/
6) Other medical considerations (safety and fit)
Your overall health also matters. Certain conditions may influence eligibility or require extra planning—for example, significant cardiopulmonary disease, bleeding disorders, active infections, neuromuscular disease affecting the airway, inability to operate or comply with device use, or prior upper-airway surgeries that change anatomy. This is why candidacy is determined by a full evaluation, not self-screening alone.
— Summary: Candidacy requires the right diagnosis, CPAP documentation, BMI within policy, compatible anatomy on DISE, and medical safety for implantation. —
Contraindications & Common Reasons Patients Are Denied
Common reasons for denial include:
- Predominantly central sleep apnea or a high central/mixed component
- DISE pattern not compatible (e.g., complete concentric palatal collapse)
- BMI above the plan’s coverage threshold
- OSA severity not in the range required by criteria/policy
- Missing documentation of CPAP intolerance (e.g., no compliance report)
Tip: A denial for Inspire therapy doesn’t mean you’re out of options—it often means a different treatment path is a better fit right now.
— If Inspire isn’t a fit today, your team can help map the best alternative path forward. —
Special Population: Inspire for Teens With Down Syndrome (Ages 13–18)
Inspire is also approved for certain pediatric patients with Down syndrome, typically ages 13–18, who have severe OSA and haven’t been helped by other treatments (including CPAP and adenotonsillectomy where appropriate). Criteria and workflow differ from adult evaluation.
Source: https://www.inspiresleep.com/en-us/qualification-requirements/
— For Down syndrome teens with severe OSA, Inspire may be considered when other treatments haven’t worked. —
Step-by-Step — What to Expect During an Inspire Candidacy Evaluation
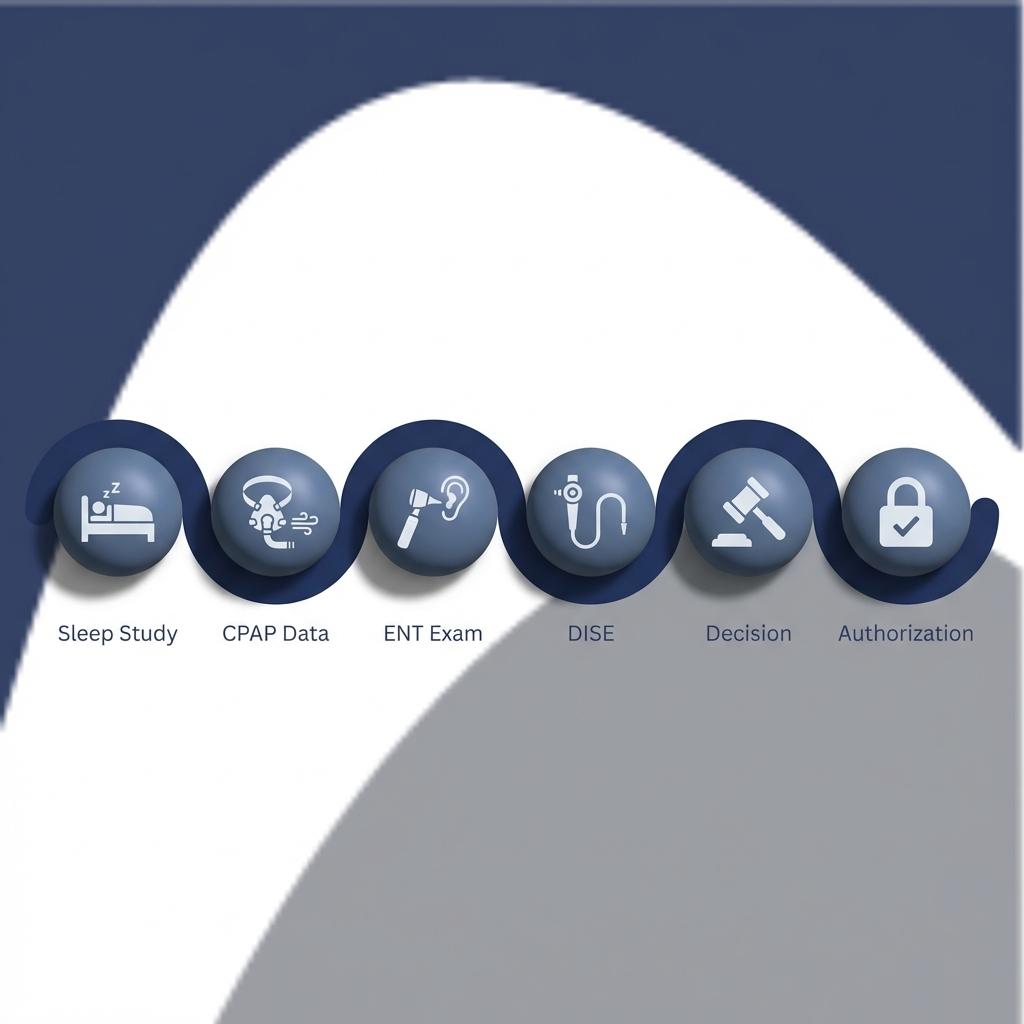
At Sleep and Sinus Centers of Georgia, an Inspire candidacy workup commonly includes:
Step 1: Review your sleep study
Your report helps confirm:
- AHI severity
- Oxygen levels
- Obstructive vs central components
If your study is older or incomplete for current requirements, your clinician may recommend repeating it—especially if symptoms or weight have changed.
Step 2: Document CPAP attempts
Helpful items include:
- A CPAP compliance download (hours/night, nights/week)
- A short history of masks tried, pressure changes, humidification, and comfort settings
Even a short list like “nasal mask → full-face mask → pressure adjustment → heated humidity” can make the record clearer and speed up authorization.
Step 3: ENT airway exam
An in-office exam can evaluate nasal and throat anatomy that may affect your sleep breathing and treatment options.
Step 4: DISE procedure and results
DISE is often the deciding step because it confirms whether your collapse pattern fits the device’s indications.
Step 5: Shared decision-making
If you qualify, you’ll review practical considerations: how the device is used, expected benefits, limitations, and follow-up. This is also the time to talk through personal priorities—quieting snoring for a partner, reducing daytime fatigue, or improving sleep continuity.
Step 6: Insurance authorization process and timelines
Coverage and timelines vary. For logistics and costs, see: https://sleepandsinuscenters.com/blog/inspire-sleep-apnea-device-cost-qualifications-and-20260129051011
— Expect a structured process: confirm diagnosis, document CPAP issues, assess anatomy with DISE, and work through coverage steps. —
Treatments & Alternatives if You Don’t Qualify (or Don’t Want an Implant)
Not qualifying for Inspire doesn’t mean you’re stuck. Evidence-based options may include:
- Improving CPAP tolerance (mask refitting, comfort adjustments, humidity, addressing nasal blockage)
- Oral appliance therapy for appropriate candidates
- Positional therapy, weight management strategies, and reducing alcohol near bedtime
- Targeted treatment of nasal obstruction to improve sleep and/or CPAP comfort
- Surgical options when anatomy suggests a different approach
For a patient-friendly breakdown, see: https://sleepandsinuscenters.com/blog/evidence-based-cpap-alternatives-that-actually-wor-20260129191420
Note: Many alternatives require evaluation to confirm suitability and safety for your specific situation.
— The right alternative depends on your anatomy, goals, and health profile—your care team will guide individualized choices. —
Lifestyle Tips That Support Any Sleep Apnea Treatment Plan
- Maintain healthy routines around weight, exercise, and sleep schedule
- Reduce alcohol near bedtime, which can worsen airway collapse
- Support nasal breathing (allergy control and chronic congestion management can matter)
- Track symptoms over time (snoring intensity, witnessed apneas, daytime alertness)
— Small, steady lifestyle changes can enhance the effectiveness of any OSA treatment. —
FAQs About Inspire Therapy Candidacy
What AHI qualifies for Inspire therapy?
In general, Inspire is considered for moderate to severe OSA. Practically, that means an AHI of 15 or greater; some payers also set an upper AHI limit. Your specific sleep study (home or lab) and policy determine the exact thresholds.
What counts as CPAP intolerance?
Commonly used definitions include inability to use CPAP ≥4 hours per night on >5 nights per week, or inability/unwillingness to use CPAP despite genuine attempts to make it work. Documentation (especially compliance data) is often essential.
Source: https://professionals.inspiresleep.com/en-us/indications-and-contraindications/
Is there a strict BMI cutoff?
It depends. Clinical programs may evaluate candidates across a range of BMIs, but insurers may apply stricter thresholds (often low-to-mid 30s). Discuss healthy weight strategies with your clinician to optimize candidacy if needed.
Sources: https://professionals.inspiresleep.com/en-us/indications-and-contraindications/ and https://www.brighamandwomensfaulkner.org/programs-and-services/sleep-medicine-and-endocrinology/sleep-medicine-inspire
What is DISE and is it required?
DISE (drug-induced sleep endoscopy) is a sedation-based airway evaluation used to confirm your collapse pattern and rule out contraindications like complete concentric palatal collapse. It’s commonly part of candidacy.
Source: https://professionals.inspiresleep.com/en-us/indications-and-contraindications/
Can Inspire help if my main issue is snoring?
Inspire is intended for diagnosed obstructive sleep apnea, not simple snoring alone. A sleep study is the usual way to confirm a diagnosis.
How long does approval take and will insurance cover it?
Timelines vary depending on required testing, documentation, and pre-authorization. For costs and coverage insights, see: https://sleepandsinuscenters.com/blog/inspire-sleep-apnea-device-cost-qualifications-and-20260129051011
— Your AHI, CPAP history, DISE findings, BMI, and overall health all factor into approval and timing. —
Call to Action — Next Steps if You Think You Might Qualify
Bring these items to your consultation
- Your most recent sleep study report
- CPAP compliance report (if available) and a list of masks/settings tried
- Current weight/BMI and key medical history
Schedule an evaluation
If you’d like to explore Inspire therapy candidacy (or confirm the best alternative), book an appointment with Sleep and Sinus Centers of Georgia: https://sleepandsinuscenters.com/appointments
Learn more about our practice: https://www.sleepandsinuscenters.com/
Sources
- Inspire Sleep — Qualification Requirements: https://www.inspiresleep.com/en-us/qualification-requirements/
- Inspire Professionals — Indications & Contraindications: https://professionals.inspiresleep.com/en-us/indications-and-contraindications/
- Brigham and Women’s Faulkner Hospital — Inspire overview (BMI/eligibility context): https://www.brighamandwomensfaulkner.org/programs-and-services/sleep-medicine-and-endocrinology/sleep-medicine-inspire
- Sleep and Sinus Centers of Georgia — Inspire device cost/qualifications: https://sleepandsinuscenters.com/blog/inspire-sleep-apnea-device-cost-qualifications-and-20260129051011
- Sleep and Sinus Centers of Georgia — Inspire HNS overview: https://sleepandsinuscenters.com/blog/inspire-hypoglossal-nerve-stimulation-a-101-guide-to-sleep-apnea-treatment
- Sleep and Sinus Centers of Georgia — AHI score explainer: https://sleepandsinuscenters.com/blog/ahi-score-explained-understanding-your-sleep-apnea-severity
- Sleep and Sinus Centers of Georgia — CPAP alternatives: https://sleepandsinuscenters.com/blog/evidence-based-cpap-alternatives-that-actually-wor-20260129191420
Disclaimer
This article is for educational purposes only and is not medical advice. Please consult a qualified healthcare provider for diagnosis and treatment.
Don’t let allergies slow you down. Schedule a comprehensive ENT and allergy evaluation at Sleep and Sinus Centers of Georgia. We’re here to find your triggers and guide you toward lasting relief.







