Inspire Sleep Apnea Device Cost, Qualifications, and Results
If you’ve been diagnosed with obstructive sleep apnea (OSA) and you’ve tried CPAP but can’t sleep with it, you may have heard about Inspire therapy—an implanted option designed to treat OSA without a mask. This guide breaks down Inspire Sleep Apnea Device Cost, typical insurance coverage, Inspire sleep apnea qualifications, expected outcomes, and what the process looks like from evaluation through long-term follow-up.
What Is Inspire Therapy for Sleep Apnea?
The problem: CPAP works, but many people can’t tolerate it
CPAP is still considered a gold-standard treatment for OSA because it can be very effective—when you can actually use it. But real life matters: mask leaks, pressure discomfort, dryness, noise, or simply being unable to sleep connected to equipment can make CPAP hard to use consistently.
A common scenario looks like this: someone starts strong, then gradually uses CPAP less and less because they wake up pulling the mask off, or they dread bedtime because the setup feels stressful. When CPAP isn’t used reliably, results often fall short—so people start looking for alternatives that fit their sleep style, not just their diagnosis.
What Inspire is (and isn’t)
Inspire therapy is an implanted treatment for moderate to severe obstructive sleep apnea in people who cannot use CPAP effectively. It uses hypoglossal nerve stimulation to help keep your airway open during sleep. Think of it like a “gentle timing cue” for the muscles that help keep your airway from collapsing—rather than pressurized air from a mask.
It’s not a medication, not a mouthguard, and not a “snoring fix” for people without sleep apnea. (Source: https://www.inspiresleep.com/en-us/qualification-requirements/)
For a deeper overview, see our supporting article: Inspire implant basics (educational resource): https://sleepandsinuscenters.com/blog/inspire-implant-basics-a-guide-to-hypoglossal-nerve-stimulation-hns-therapy
What this guide covers
- Total cost vs. what patients often pay with insurance
- Insurance coverage details (including Medicare/VA)
- Qualifications and evaluation steps
- Inspire implant results and realistic expectations
- Risks, downsides, and alternatives
- Practical next steps
- This article is not a substitute for medical evaluation
Inspire is a mask-free option for selected adults who can’t benefit from CPAP and want a therapy aligned with their sleep routine.
Sleep Apnea Basics (Symptoms, Causes, and Why Treatment Matters)
Common symptoms of obstructive sleep apnea
OSA often shows up as:
- Loud, persistent snoring
- Choking or gasping during sleep
- Witnessed pauses in breathing
- Daytime sleepiness or fatigue
- Morning headaches
- Trouble with focus, memory, or mood
Some people are surprised by their diagnosis because their “main symptom” isn’t snoring—it’s brain fog, irritability, or needing naps to get through the day. If any of this sounds familiar, you’re not alone.
What causes OSA
OSA occurs when the upper airway narrows or collapses during sleep. Contributing factors can include airway anatomy, weight, alcohol or sedative use, nasal obstruction, and age-related changes in muscle tone.
One way clinicians often explain it: during sleep, the tissues of the throat relax; in OSA, that relaxation is enough to partially or fully block airflow, leading to repeated breathing disruptions.
Why treating OSA is important
Untreated OSA can affect both quality of life and long-term health. Many people pursue treatment not only for better sleep and energy, but also because OSA has known associations with cardiometabolic and safety risks (like drowsy driving).
If you’re not sure how your diagnosis is classified, this resource can help: AHI score explained (educational resource): https://sleepandsinuscenters.com/blog/ahi-score-explained-understanding-your-sleep-apnea-severity
Treating OSA can improve daily function now and support long-term health over time.

How Inspire Works (Patient-Friendly Explanation)
Hypoglossal nerve stimulation in plain language
The hypoglossal nerve helps control tongue movement. During sleep, the tongue and surrounding tissues can fall back and narrow the airway. Inspire delivers gentle, timed stimulation that moves the tongue forward to help keep breathing passages open.
A helpful analogy: if your airway is like a soft tunnel that can sag during sleep, Inspire is designed to support the “front end” so airflow has more room—without using a mask to push air in.
What the device includes
Inspire therapy typically involves:
- An implanted stimulation component
- A breathing-sensing component
- A small implanted power unit
- A handheld remote you use at bedtime to turn therapy on/off (and to pause it if needed)
Many patients like the bedtime routine: remote on, fall asleep, and the system does the work in the background. A clinician might describe it simply as, “You’re in control at night, and we fine-tune comfort over time.”
Who Inspire is designed for
It’s intended for adults with moderate to severe OSA who haven’t been able to benefit from CPAP. (Source: https://www.inspiresleep.com/en-us/qualification-requirements/)
Inspire coordinates with your natural breathing to help keep the airway open while you sleep.

Inspire Sleep Apnea Device Cost (Total Cost vs. What Patients Usually Pay)
Typical total procedure cost
The total price for the device, surgery, and associated care is often reported in the $30,000–$40,000 range. (Sources: https://www.inspiresleep.com/en-us/cost-and-insurance/ | https://www.verywellhealth.com/how-much-do-different-sleep-apnea-treatments-cost-4177858)
This is the “sticker price”—but it’s not necessarily what you’ll personally pay.
Why the sticker price isn’t what most insured patients pay
According to Inspire, many insured patients report $0 to under ~$1,000 out-of-pocket, depending on plan design. Out-of-pocket costs vary widely based on deductible status, coinsurance, out-of-pocket maximums, and network coverage, so your experience may differ. (Source: https://www.inspiresleep.com/en-us/cost-and-insurance/)
Here’s a concrete way to think about it: two patients can have the same device and surgery, but if one has already met their deductible (or has a low out-of-pocket maximum), their personal cost may be far lower than someone early in the plan year with a high deductible.
What affects your out-of-pocket cost
Common cost variables include:
- Where you are in your deductible for the year
- Outpatient vs. inpatient billing and facility fees
- Whether the surgeon, facility, and anesthesia are in-network
- Prior authorization requirements and documentation needs
Questions to ask your insurance plan before scheduling
Consider asking:
- Is Inspire covered for my diagnosis and plan?
- Is prior authorization required?
- Do you need documentation of CPAP failure/intolerance?
- What will my deductible/coinsurance apply to?
- Are the facility, surgeon, and anesthesia providers in-network?
- What is my remaining out-of-pocket maximum?
The “sticker price” rarely reflects your actual cost—your insurance details and timing in the plan year matter most.

Insurance Coverage for Inspire (Medicare, VA, and Commercial Plans)
Is Inspire covered by insurance?
Inspire reports coverage by most major insurers, including Medicare and VA, for people who meet medical criteria and FDA indications. (Source: https://www.inspiresleep.com/en-us/cost-and-insurance/)
Medicare and VA considerations
Coverage typically hinges on documented medical necessity and meeting the published qualification requirements. (Source: https://www.inspiresleep.com/en-us/cost-and-insurance/)
Prior authorization and documentation you may need
Common documentation includes:
- Sleep study results and AHI severity
- Evidence you could not use CPAP effectively (intolerance/failure)
- BMI
- Airway evaluation findings
(Source: https://www.inspiresleep.com/en-us/qualification-requirements/)
A practical tip: keep a clear timeline of your CPAP experience (mask trials, pressure changes, comfort issues). That history can make insurance review smoother because it shows you made a real effort.
Insurance approval depends on meeting criteria and having clear documentation of CPAP intolerance and OSA severity.
Inspire Qualifications (Who Is a Good Candidate?)
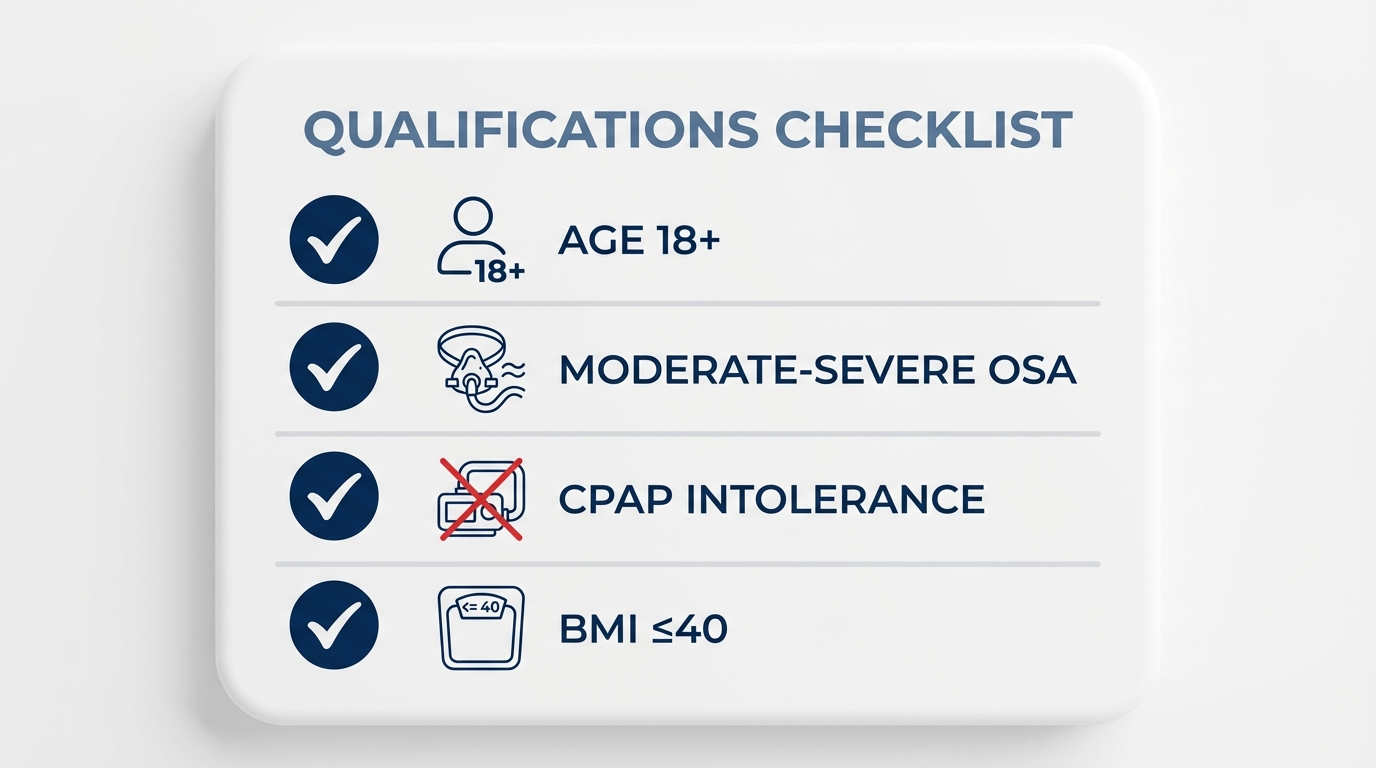
Core eligibility requirements
While exact criteria can vary by insurer, commonly listed requirements include:
- Age 18+
- Moderate to severe OSA
- Unable to benefit from CPAP
- BMI often ≤ 40 (some insurers require lower)
(Source: https://www.inspiresleep.com/en-us/qualification-requirements/)
These criteria are central to Inspire sleep apnea qualifications and are usually reviewed early in the process.
What “can’t tolerate CPAP” usually means
“CPAP intolerance” often refers to issues like:
- Mask discomfort or skin irritation
- Persistent leaks despite refitting
- Claustrophobia
- Pressure intolerance
- Inability to sleep with CPAP long enough to get benefit
Importantly, CPAP intolerance is a clinical judgment and requires appropriate documentation for insurance approval. In real terms, “I own a CPAP” isn’t the same as “I can use CPAP consistently.”
Other medical factors that may matter
Candidacy also depends on airway anatomy and other health considerations that your sleep and ENT team evaluates. Not everyone with OSA is a fit for hypoglossal nerve stimulation.
One ENT-style way of summarizing this: “Severity and CPAP intolerance get you in the door; your airway evaluation helps confirm the approach makes sense for your anatomy.”
Quick self-check: signs you may want an Inspire consultation
You may be ready to discuss Inspire if:
- You have documented OSA (especially moderate–severe)
- Symptoms persist (sleepiness, snoring, poor sleep quality)
- You’ve made a real effort with CPAP troubleshooting but still can’t use it reliably
A good Inspire candidate has qualifying OSA, documented CPAP intolerance, and suitable airway anatomy.
The Evaluation Process (What to Expect Before You’re Approved)
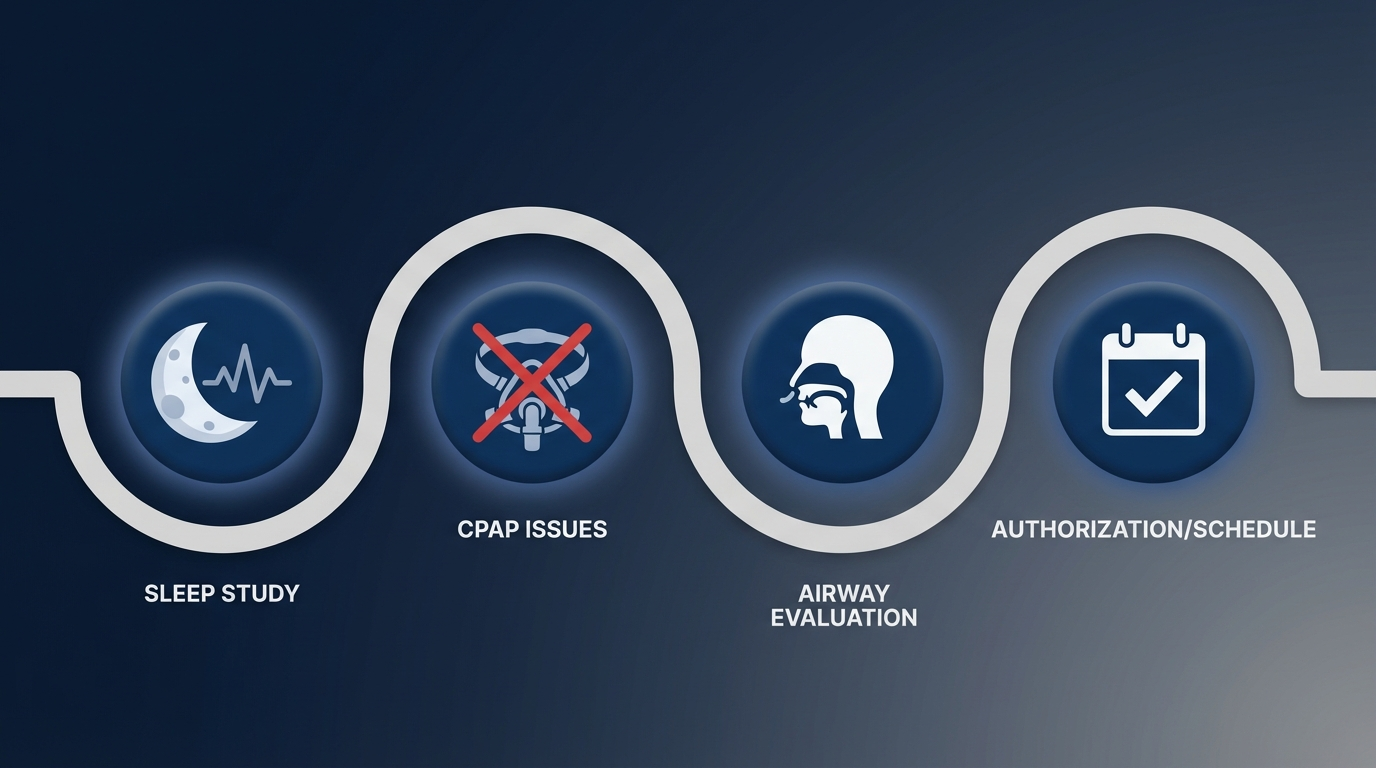
Step 1 — Confirm diagnosis and severity
A sleep study is reviewed to confirm OSA type and severity (often via AHI). This helps ensure the therapy is being considered for the right condition—Inspire is designed for obstructive events, not other sleep-related breathing disorders.
Step 2 — Document CPAP intolerance/failure
Your history with CPAP matters. Insurance commonly requires documentation showing you tried CPAP but couldn’t use it effectively. Your clinic can help translate your experience (mask issues, pressure problems, inability to sleep) into the documentation insurers look for.
Step 3 — Airway evaluation
An ENT evaluation helps determine whether your airway anatomy is compatible with Inspire therapy.
Step 4 — Insurance authorization and scheduling
After your clinical evaluation, the team typically submits information for authorization. Timelines vary—delays often come from missing documentation or insurer requests for additional records.
A clear sleep study, documented CPAP issues, and an airway assessment form the backbone of Inspire approval.
Inspire Results (Effectiveness and Realistic Expectations)
How effective is Inspire for OSA control?
In appropriately selected patients, many clinical programs report high success rates, with some citing over 90% of patients achieving significant control of their sleep apnea. “Control” generally refers to substantial reductions in apnea events and symptom improvement, but individual responses vary. (Source: https://www.nmhs.net/Blog/New-Device-Revolutionizing-Sleep-Apnea-Treatment)
What “results” usually means (not just AHI)
- Reduced snoring
- Fewer breathing disruptions
- Better sleep continuity
- Improved daytime alertness and energy
A patient-style way to describe the goal is: “I want quieter nights and more functional days.”
When patients typically notice improvement
Improvement is often not immediate. Many people notice changes after: 1) healing from surgery, 2) device activation, and 3) a period of adjustment (“titration”) to optimize settings.
This pacing is important for expectations. It’s less like flipping a switch and more like getting a prescription tuned to the right dose—comfort and effectiveness both matter.
What results are not guaranteed
Responses vary. Some people get major improvement; others may see partial improvement and need additional support (such as lifestyle changes or adjunct therapies).
Expect meaningful improvements over weeks to months as settings are optimized, with results varying by individual.
Risks, Downsides, and Long-Term Considerations
Common side effects
Potential side effects may include temporary soreness, discomfort near implant sites, or tongue sensation changes—especially early on.
Revision surgery and device issues
As with any implanted therapy, some patients may need additional procedures due to device issues, discomfort, or suboptimal results.
Battery life and future replacement
The battery does not last forever. Battery replacement involves minor surgery with associated recovery. Discuss long-term device maintenance, expected battery lifespan, and replacement logistics—including billing and downtime—with your care team as part of your decision-making process.
Plan for the full life cycle of the device, including potential adjustments and eventual battery replacement.
Inspire Procedure and Recovery (Patient-Friendly Walkthrough)
The surgery (high-level overview)
Inspire implantation is a surgical procedure performed by an ENT surgeon. Components are placed under the skin and connected so therapy can coordinate with your breathing.
Recovery timeline
Recovery experiences vary, but many people plan for a short-term recovery period with activity restrictions. Your surgeon will provide personalized instructions.
Activation and titration (“dialing it in”)
Inspire is typically activated after healing, then adjusted over follow-up visits to find settings that balance comfort and effectiveness. Many patients describe it as a brief learning curve while the care team optimizes settings.
Expect a straightforward day-to-day routine with several follow-ups to fine-tune comfort and effectiveness.
Alternatives to Inspire (Other Treatments for OSA)
CPAP optimization (before giving up)
Before moving on, many people benefit from:
- Mask refitting (style/size changes)
- Humidification tweaks
- Pressure adjustments
If CPAP is getting in the way, this may help: Is your CPAP machine getting in the way? (educational resource): https://sleepandsinuscenters.com/is-your-cpap-machine-getting-in-the-way
Oral appliance therapy
Custom oral appliances can be a strong CPAP alternative for sleep apnea in selected patients—especially some mild to moderate cases. Related read: Oral appliance vs CPAP (educational resource): https://sleepandsinuscenters.com/blog/oral-appliance-vs-cpap-which-is-right-for-you
Positional therapy
For position-dependent OSA, avoiding back-sleeping can reduce events for some people.
Weight management and lifestyle changes
Weight changes can influence airway anatomy and OSA severity and may improve outcomes alongside any primary therapy. Related read: Weight loss and sleep apnea (educational resource): https://sleepandsinuscenters.com/blog/weight-loss-and-its-impact-on-sleep-apnea-key-benefits-and-insights
Other surgical options
In some cases, anatomy-focused procedures may be considered, depending on the cause of obstruction.
If Inspire isn’t the right fit, there are other evidence-based options that can be tailored to your needs.
Lifestyle Tips That Can Improve Results (With or Without Inspire)
Sleep position strategies
Side-sleeping may help some patients, particularly if events worsen on the back. Even small changes—like using pillows to stay off your back—can be worth discussing with your clinician.
Alcohol and sedative avoidance
Alcohol and sedatives can relax airway muscles and worsen collapsibility in some people. If snoring or events spike after drinking, that pattern is a useful clue to share at follow-ups.
Weight, exercise, and cardiometabolic health
Healthy routines can support better sleep and overall health. For more: Weight loss and sleep apnea (educational resource): https://sleepandsinuscenters.com/blog/weight-loss-and-its-impact-on-sleep-apnea-key-benefits-and-insights
Nasal breathing support
Addressing chronic congestion or allergies may improve comfort and sleep quality, regardless of your primary treatment.
Small daily habits—sleep position, alcohol timing, weight management, and nasal care—can amplify the benefits of any OSA therapy.
FAQs
1) How much does the Inspire sleep apnea device cost with insurance?
While total charges may be high, many insured patients report paying $0 to under ~$1,000, depending on deductible and plan design. Out-of-pocket costs vary widely based on your benefits, remaining deductible, and in-network status, so your experience may differ. (Source: https://www.inspiresleep.com/en-us/cost-and-insurance/)
If you’re comparing Inspire Sleep Apnea Device Cost scenarios, your benefits and in-network status matter most.
2) Is Inspire covered by Medicare or the VA?
Often yes—when medical criteria and documentation requirements are met. (Source: https://www.inspiresleep.com/en-us/cost-and-insurance/)
3) What BMI do you need to qualify for Inspire?
Commonly ≤ 40, though some insurers require a lower BMI cutoff. (Source: https://www.inspiresleep.com/en-us/qualification-requirements/)
4) How successful is Inspire for sleep apnea?
Outcomes can be strong in well-selected patients, and some programs report high control rates, generally meaning substantial reductions in apnea events and symptoms. Individual results vary. (Source: https://www.nmhs.net/Blog/New-Device-Revolutionizing-Sleep-Apnea-Treatment)
5) Can you still snore with Inspire?
Yes. Many people snore less, but snoring can persist depending on anatomy, sleep position, alcohol use, and other factors.
6) Can Inspire replace CPAP completely?
For many people, Inspire may serve as an alternative to CPAP. However, some patients might still require additional or adjunctive therapies for optimal sleep apnea control.
7) What happens if I don’t qualify for Inspire?
Not qualifying doesn’t mean you’re out of options—CPAP troubleshooting, oral appliances, lifestyle changes, positional therapy, or other procedures may be considered.
8) How do I start the process?
Typical next steps include a sleep study review, a candidacy consultation, airway evaluation, and insurance authorization.
Most questions boil down to eligibility, costs, expected results, and your personal preferences for therapy.
Conclusion — Is Inspire Worth It?
Best candidates tend to share 3 traits
People who do best with Inspire often have: 1) Moderate to severe OSA, 2) CPAP intolerance/failure, and 3) Eligibility based on anatomy and insurer/FDA criteria.
Key takeaway on cost
The Inspire Sleep Apnea Device Cost is often quoted in the $30,000–$40,000 range, but insurance coverage can make the patient portion far more manageable. (Source: https://www.inspiresleep.com/en-us/cost-and-insurance/)
Call to action
If you’re wondering whether you meet Inspire sleep apnea qualifications, the most efficient next step is a consultation to review your sleep study, CPAP history, and insurance benefits so you can get a personalized estimate and realistic expectations. To book an appointment, visit https://www.sleepandsinuscenters.com/
If CPAP isn’t workable for you, Inspire may be a practical, mask-free path to better sleep and daytime energy.
Disclaimer: This article is for educational purposes only and is not medical advice. Please consult a qualified healthcare provider for diagnosis and treatment.
Don’t let allergies slow you down. Schedule a comprehensive ENT and allergy evaluation at Sleep and Sinus Centers of Georgia. We’re here to find your triggers and guide you toward lasting relief.







