Sleep Apnea Surgery Options in Atlanta: Complete Guide to Treatment and Recovery
If you’ve been diagnosed with obstructive sleep apnea (OSA) and CPAP hasn’t been a good fit, you may be wondering what sleep apnea surgery options in Atlanta look like—and what recovery and cost might involve. This guide walks through the most common procedures, who they’re designed to help, and how to think about next steps in a patient-friendly way.
A helpful way to picture OSA is this: your airway is like a flexible tube. During sleep, the “tube” can get pinched at one spot (or several), and breathing becomes interrupted. Surgery is less about a single “magic fix” and more about opening or stabilizing the specific pinch points that show up in your anatomy and sleep study results.
Quick Overview (TL;DR)
- When surgery is considered: often when OSA is moderate to severe, when CPAP isn’t tolerated, or when anatomy makes non-surgical treatment difficult.
- Main categories of sleep apnea surgery options in Atlanta:
- Soft-tissue throat procedures (like palate surgery)
- Nasal surgery (to improve airflow and CPAP comfort)
- Tongue/tongue-base procedures
- Skeletal surgery (jaw advancement)
- Implantable nerve stimulation (Inspire)
- Weight-loss (bariatric) surgery in select cases
- Cost and insurance: pricing varies widely by procedure and setting. A broad estimate often cited is ~$6,400 to $100,000+ depending on what’s done and how complex the case is. Insurance may cover surgery when medically necessary, typically with pre-authorization. [1][5]

What Is Obstructive Sleep Apnea (OSA)?
Why OSA happens (simple explanation)
OSA happens when the airway repeatedly narrows or collapses during sleep, reducing airflow. This can occur at different “levels” of the airway—such as the nose, the soft palate, the tonsil region, or behind the tongue.
Some people have one main collapse site; others have a “multi-level” pattern. That’s one reason two patients can have the same AHI but need very different treatment plans.
Why treating OSA matters
Untreated OSA is linked with quality-of-life issues like poor sleep and daytime fatigue, and it’s also associated with longer-term health concerns (including cardiovascular strain in some people). Treatment is about improving breathing at night, sleep quality, and overall health.
“A lot of patients tell us they didn’t realize how much OSA affected them until they start sleeping—and thinking—more clearly.” —Clinician perspective (commonly heard in sleep clinics)
Effective OSA care starts by identifying exactly where the airway collapses so treatment targets the right spot.
Common Sleep Apnea Symptoms (When to Get Evaluated)
Nighttime symptoms
- Loud, frequent snoring
- Choking or gasping during sleep
- Witnessed pauses in breathing
- Restless sleep or frequent awakenings
Daytime symptoms
- Morning headaches
- Brain fog or trouble concentrating
- Irritability or mood changes
- Excessive sleepiness
- Fatigue and concerns about high blood pressure
If these symptoms sound familiar, consider talking with a sleep specialist about evaluation and treatment options. You can also learn more about snoring and sleep apnea treatment at Sleep and Sinus Centers of Georgia: https://sleepandsinuscenters.com/snoring-sleep-apnea-treatment
If symptoms sound familiar, get evaluated—testing guides the right plan more reliably than guesswork.
Causes & Risk Factors (Why Some People Need Surgery)
Anatomy-related causes (common “block points”)
Different structures can contribute to blockage, including:
- Nose: deviated septum, enlarged turbinates, chronic congestion
- Throat/soft palate: elongated soft palate/uvula, tissue crowding
- Tonsils: enlarged tonsils (yes, even in adults)
- Tongue base and jaw structure: tongue relaxing backward, smaller/lower jaw position in some people
A concrete example: one patient may breathe well through the nose but collapse at the palate (throat-focused approach). Another may have significant nasal blockage that makes CPAP feel unbearable (nasal-focused approach to improve airflow and comfort).
Health and lifestyle contributors
- Weight gain or obesity
- Alcohol or sedatives (which relax airway muscles)
- Back-sleeping (positional worsening for some)
- Allergies or chronic nasal inflammation limiting airflow
Surgery is usually considered when anatomy plays a meaningful role—especially when improving airflow could reduce events or improve tolerance of other therapies.
When anatomy is a major driver, a targeted surgical plan can reduce collapse and support other therapies.
How Sleep Apnea Is Diagnosed (Before Surgery Is Even on the Table)
Sleep study options (home vs. lab)
OSA is diagnosed using a sleep study, either at home or in a sleep lab, depending on your symptoms and medical history. The best test depends on complexity and what your clinician needs to measure.
A practical example: a straightforward snoring + suspected OSA case may start with a home test, while more complex symptoms or medical conditions may steer you toward an in-lab study.
Understanding severity (AHI and what it means)
Severity is commonly described with the Apnea-Hypopnea Index (AHI), which reflects how many breathing disruptions occur per hour of sleep. For a simple breakdown, see AHI score explained: https://sleepandsinuscenters.com/blog/ahi-score-explained-understanding-your-sleep-apnea-severity
Many clinicians also use AHI ranges (mild/moderate/severe) as a shared language for expectations—especially when discussing whether surgery is meant to reduce severity, improve symptoms, or support CPAP tolerance.
Airway evaluation (why ENT exams matter)
Because sleep apnea surgery options in Atlanta are highly dependent on where the airway collapses, an airway exam is often part of a surgical evaluation. This may include:
- Nasal exam and endoscopy
- Imaging in select cases
- Drug-induced sleep endoscopy (DISE) in some patients, to better localize collapse patterns
Think of DISE like “watching the airway during sleep conditions,” which can help your team avoid guessing and focus on the most relevant collapse sites.
Testing plus airway localization lays the groundwork for a plan that matches your anatomy.

When Is Sleep Apnea Surgery Recommended?
- CPAP isn’t tolerated or isn’t effective
- Oral appliance therapy doesn’t work or isn’t appropriate
- Moderate–severe OSA is present and anatomy suggests surgery could help [5]
Who may not be a good candidate
Surgery isn’t one-size-fits-all. Some people may have medical risks that require extra planning, or airway patterns that respond better to non-surgical treatment. It’s also common for surgical care plans to involve more than one procedure (for example, nasal surgery plus another airway procedure), depending on the findings.
A reassuring point: “Not a candidate” for one procedure doesn’t mean “no options.” It often means you need a different match.
Surgical candidacy depends on both your sleep study and the specific anatomy driving your OSA.
Non-Surgical Treatments to Try First (and Why They Sometimes Fail)
CPAP / APAP / BiPAP basics
Positive airway pressure devices keep the airway open by providing a steady flow of air. They’re highly effective for many patients—but comfort, mask fit, pressure tolerance, and nasal blockage can make them hard to use consistently.
If CPAP feels like “too much air,” it may not be a willpower problem—it may be a nasal airflow or pressure issue that can sometimes be addressed.
Oral appliances
Custom oral appliances may help selected patients (often mild to moderate OSA, or specific anatomy). They can be a good alternative when CPAP isn’t tolerated.
Lifestyle and positional therapy
Weight management, reducing alcohol near bedtime, and positional therapy (avoiding back sleeping) can improve OSA severity for some people.
Why nasal obstruction can sabotage CPAP comfort
If nasal breathing is difficult, CPAP can feel more uncomfortable and “forceful,” which sometimes reduces adherence. In these cases, nasal procedures may be discussed as part of an overall treatment plan—even if they aren’t expected to cure OSA by themselves. [5]
Try evidence-based non-surgical options first; surgery is usually reserved for anatomy-driven, persistent OSA.
Sleep Apnea Surgery Options in Atlanta (Main Procedures Explained)
A key idea: your best option depends on where your airway collapses. Many people do best with a combined approach tailored to their anatomy and sleep study results. Below are the most common categories used in modern obstructive sleep apnea surgery Atlanta treatment pathways. [5]
1) Soft Tissue Surgery (Throat/Palate)
UPPP (Uvulopalatopharyngoplasty)
- What it targets: soft palate/uvula area (and sometimes adjacent tissues)
- Who may benefit: people with palate-related obstruction patterns
- Recovery snapshot: sore throat is common early on; eating/drinking comfort can be temporarily affected
- Tradeoffs: results can vary by anatomy, and recovery can be more uncomfortable than nasal procedures; some patients may experience temporary swallowing difficulties or voice changes [5]
Tonsillectomy (adults) and related procedures
When tonsils are enlarged and contributing to airway crowding, tonsil surgery may be part of a plan (either alone or combined with palate procedures).
A simple example: if tonsils are physically narrowing the throat, removing them can create more space—especially when tonsil size is clearly part of the “crowding” seen on exam.
2) Jaw Advancement Surgery (Skeletal Surgery)
MMA (Maxillomandibular Advancement)
Jaw advancement surgery for sleep apnea (often called MMA) moves the upper and lower jaws forward to enlarge airway space.
- What it does: expands the skeletal framework around the airway
- When considered: often for moderate–severe OSA, especially when jaw structure contributes to a smaller airway [1]
- Recovery snapshot: typically a longer recovery and higher complexity than soft-tissue or nasal surgery, with more swelling and diet restrictions early on
Because MMA changes the “frame” around the airway, it’s often discussed when the limiting factor isn’t just soft tissue—it’s the available space.
3) Nasal Surgeries (Improve Nasal Airflow and CPAP Tolerance)
Septoplasty (deviated septum repair)
Helps straighten the septum to improve airflow through the nose.
Turbinate reduction
Reduces enlarged turbinates (structures inside the nose) that can contribute to congestion.
Sinus procedures (when chronic sinus disease contributes)
When chronic sinus issues or inflammation contribute to ongoing blockage, sinus procedures may be considered.
Important expectation-setting: nasal surgery may not “cure” OSA on its own, but it can improve breathing and may make CPAP or other therapies easier to use. [5]

4) Tongue & Tongue-Base Procedures
Tongue reduction / tongue-base surgery (overview)
These procedures aim to reduce collapse behind the tongue—one of the common sites of obstruction during sleep.
Genioglossus advancement (where applicable)
This approach is designed to help stabilize tongue position and reduce tongue-base collapse, improving airflow in carefully selected patients. [5]
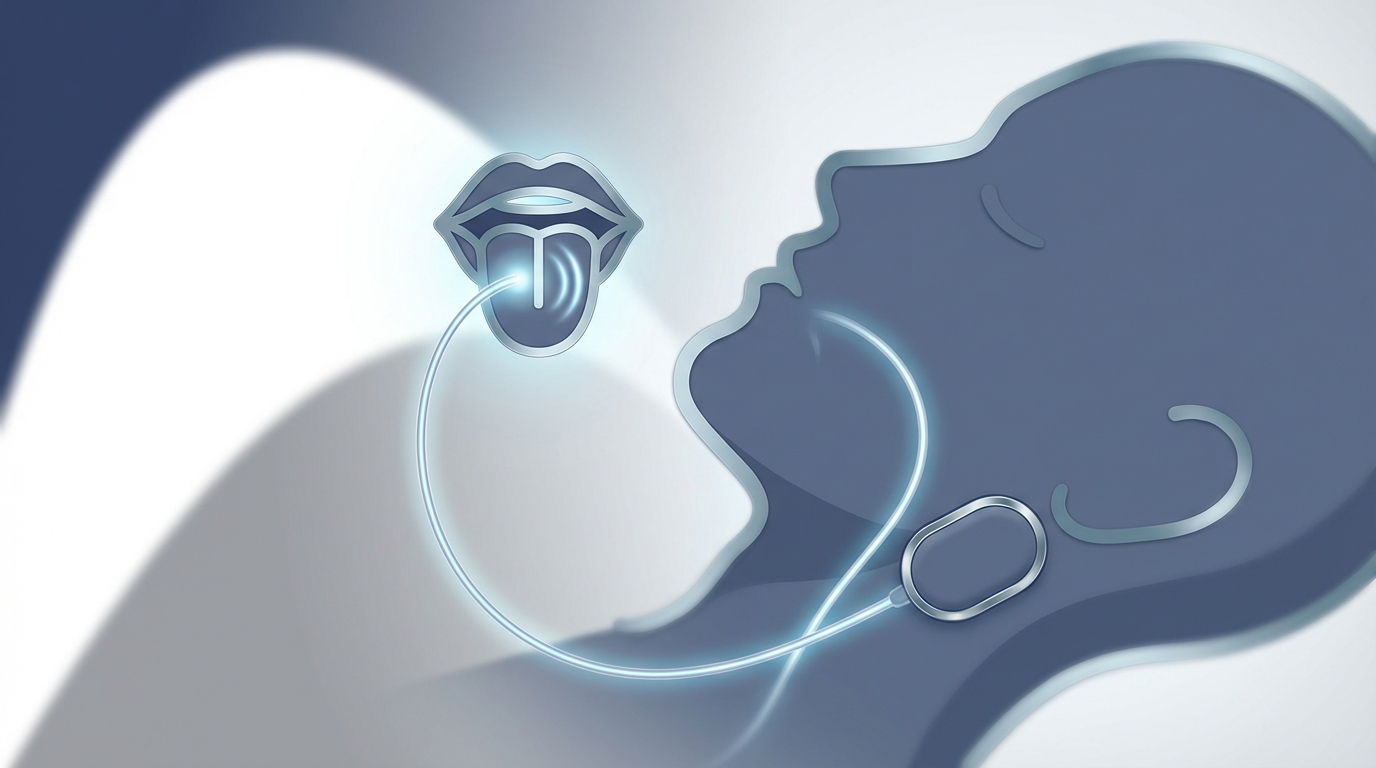
5) Hypoglossal Nerve Stimulation (Inspire)
What Inspire is
The Inspire procedure Atlanta patients ask about is an implantable system that stimulates the hypoglossal nerve during sleep to help keep the tongue from collapsing backward.
Who qualifies (typical criteria evaluated)
- CPAP intolerance
- Sleep study severity range (Inspire is FDA-approved for select adults with moderate to severe OSA who meet specific criteria)
- Anatomy evaluation to confirm the collapse pattern fits what the device treats [3][5]
For a deeper overview, see our Inspire hypoglossal nerve stimulation guide: https://sleepandsinuscenters.com/blog/inspire-hypoglossal-nerve-stimulation-a-101-guide-to-sleep-apnea-treatment
What the process looks like
A typical pathway includes evaluation → outpatient procedure → healing → device activation and fine-tuning (“titration”) over time.
Many patients like that it’s not “one-and-done”—it’s adjustable, with follow-up visits designed to dial in comfort and effectiveness. [3]
6) Weight Loss Surgery (Bariatric Surgery) for OSA
When it’s considered
When weight is a major driver of OSA and other therapies haven’t worked well, bariatric surgery may be discussed as part of a broader plan. Weight loss can reduce OSA severity in many patients, though results vary and follow-up testing remains important. [5]
The best procedure is the one that matches your collapse site; many patients benefit from a combined, stepwise plan.
Comparing Your Options (Simple Patient Decision Guide)
- Best for nasal obstruction: septoplasty/turbinate reduction ± sinus procedures
- Best for palate/soft tissue collapse: palate-focused procedures like UPPP (sometimes with tonsil surgery)
- Best for tongue-related collapse: tongue-base approaches or Inspire (depending on anatomy and eligibility)
- Best for skeletal airway limitation: MMA (jaw advancement)
- Best when weight is the main driver: structured weight-loss plan ± bariatric surgery
Questions to bring to your consult
- Where does my airway collapse (nose, palate, tongue base, multiple levels)?
- What is my AHI severity and what result is realistic for my anatomy?
- Would surgery be standalone, or combined with CPAP/oral appliance?
- What does sleep apnea surgery recovery look like for the procedure you recommend?
- What follow-up testing is planned to confirm improvement?
Go into your consult with targeted questions so the plan ties directly to your sleep study and exam.
Cost of Sleep Apnea Surgery in Atlanta + Insurance Coverage
Typical cost ranges (why it varies so much)
Sleep apnea surgery cost Atlanta can vary based on:
- The procedure type (nasal vs. implant vs. jaw surgery)
- Facility and anesthesia fees
- Whether multiple procedures are combined
- Need for follow-up studies or device programming (for Inspire)
A commonly cited overall range is ~$6,400 to $100,000+. Many straightforward, outpatient nasal or palate procedures tend to fall toward the lower end of that range, especially with insurance coverage; more complex, multi-level or skeletal surgeries and implants can cost more. Your out-of-pocket costs depend on your plan specifics and pre-authorization. [1][5]
Will insurance cover sleep apnea surgery?
Many procedures are covered when deemed medically necessary, but pre-authorization is common and criteria can be specific (especially for implants). [5]
Cost questions to ask upfront
- What’s included (surgeon, facility, anesthesia, follow-ups)?
- Will I need a repeat sleep study?
- For Inspire: what costs relate to the device, activation, and titration visits?
Ask for a written estimate and confirm pre-authorization steps early to avoid surprises.
How to Choose a Sleep Apnea Surgeon/Program in Atlanta
When exploring sleep apnea surgery options in Atlanta, look for:
- A team approach: coordination between ENT and sleep medicine, and sometimes additional specialists depending on the procedure
- Airway localization in the evaluation: an exam that identifies the likely obstruction sites (rather than guessing)
- Experience with your specific procedure: for example, Inspire, UPPP, or jaw advancement pathways
If you hear a plan that doesn’t connect your sleep study + airway findings to a specific target area, it’s reasonable to ask, “What exactly are we trying to open or stabilize?”
Choose a program that matches procedures to your anatomy and tracks outcomes with follow-up testing.
What Recovery Looks Like (Treatment & Recovery Guide)
General recovery expectations
- Temporary pain/swelling
- Some sleep disruption early on
- Short-term diet or activity changes
Many patients also appreciate setting a “recovery support plan” ahead of time (soft foods, time off work, help at home for a few days, and realistic expectations for sleep quality early on).
Recovery by procedure (brief)
- Nasal surgery: congestion, saline rinses, follow-up visits; many return to normal routines relatively quickly
- UPPP/tonsil surgery: sore throat, hydration focus, soft foods for a period of time
- MMA: longer healing timeline, swelling management, and more significant diet restrictions early on
- Inspire: incision care first, then device activation later (not turned on the day of surgery) [3]
Follow-up testing: “Did it work?”
A repeat sleep study is often recommended after healing to measure improvement and guide next steps (including whether CPAP settings can be adjusted). [5]
Plan for healing, follow your instructions closely, and confirm results with a post-treatment sleep study.

Risks, Side Effects, and Realistic Outcomes
Common risks across surgeries
Bleeding, infection, anesthesia risks, pain, and swelling are possible with most surgeries.
Procedure-specific considerations
- Throat surgery: temporary swallowing or voice changes may occur
- Inspire: implant-related risks and the need for ongoing follow-up and adjustments [3]
- MMA: numbness, bite/jaw changes, and longer recovery are commonly discussed considerations
Setting expectations
Some patients still need CPAP or oral appliance therapy afterward—sometimes at lower pressure or with improved comfort. Combination therapy can be a success, not a failure. [5]
Success means safer, better sleep—sometimes through a combination of treatments rather than a single cure.
Lifestyle Tips That Improve Results (Before and After Surgery)
- Try side-sleeping if your OSA is position-dependent
- Support metabolic health and weight management (when relevant)
- Avoid alcohol or sedatives close to bedtime if they worsen symptoms
- Maintain nasal hygiene and manage allergies to support nasal breathing
FAQs (Patient-Friendly)
Can sleep apnea be cured with surgery?
Sometimes symptoms and AHI can improve significantly, but “cure” depends on anatomy, OSA severity, and the procedure. Many people aim for meaningful reduction and better sleep quality.
Which surgery has the fastest recovery?
Nasal procedures often have a shorter recovery than throat or jaw surgeries, but the “best” surgery is the one that matches the obstruction site.
What if I can’t tolerate CPAP—does that make me a surgery candidate?
CPAP intolerance is a common reason people explore sleep apnea surgery options in Atlanta, but candidacy depends on sleep study results, anatomy, and overall health.
How do I know if Inspire is right for me?
Inspire candidacy is based on defined criteria, FDA labeling for eligible adults with moderate to severe OSA, and an anatomy evaluation to confirm the collapse pattern fits the device. [3][5]
Does insurance cover Inspire or other sleep apnea surgeries?
Coverage often depends on medical necessity and meeting criteria. Pre-authorization is common. [5]
How soon will I feel better after surgery?
Some improvements may be noticed gradually as swelling resolves and sleep stabilizes. Follow-up testing is often used to confirm results. [5]
The right questions help set realistic expectations and keep your care on track.
Next Steps (Atlanta-Area Patients)
If you’re exploring sleep apnea surgery options in Atlanta, a helpful next step is a consultation to review your sleep study, symptoms, and airway anatomy. Consider bringing:
- Prior sleep study results
- CPAP usage report (if available)
- Current medication list and relevant medical history
Ready to talk through your options and get a personalized plan? Book an appointment here: https://sleepandsinuscenters.com/appointments (learn more at https://www.sleepandsinuscenters.com/)
This article is for educational purposes only and is not medical advice. Please consult a qualified healthcare provider for diagnosis and treatment.
References
[1] https://oralsurgeonatlanta.com/procedures/sleep-apnea/
[3] https://naenta.com/ent-services/snoring-sleep/inspire-procedure-for-sleep-apnea/
[5] https://www.emoryhealthcare.org/services/sleep-center/treatments/surgical
Don’t let allergies slow you down. Schedule a comprehensive ENT and allergy evaluation at Sleep and Sinus Centers of Georgia. We’re here to find your triggers and guide you toward lasting relief.







