Sinus Headache Relief: Effective Home Remedies and Treatments
Introduction — When “Sinus Pressure” Turns Into a Headache
That heavy, aching feeling across your forehead or behind your eyes can make it hard to work, sleep, or think clearly. When sinus passages become irritated, swollen, and clogged, pressure can build—sometimes triggering a true sinus-related headache and sometimes mimicking other headache types. Major medical resources note that sinus inflammation, blocked drainage, and facial pressure often travel together, which is why symptoms can feel so intense. Not all facial pressure is a true sinus headache, though—and getting the cause right is key. (Cleveland Clinic; Mayo Clinic; Harvard Health; Houston Methodist; WebMD)
A helpful way to picture it: your sinuses are like small, air-filled rooms with narrow “drainpipes.” If the lining swells or mucus thickens, the drain can’t do its job—so pressure and discomfort build in the space.
Medical disclaimer: This article is for educational purposes only and is not medical advice. If you have severe symptoms, symptoms that are worsening, or questions about medications and underlying conditions, seek care from a qualified clinician.

Why sinus headaches feel so intense (pressure + inflammation + blocked drainage)
Your sinuses are air-filled spaces in the bones of your face. When the lining swells and mucus can’t drain normally, pressure can increase and pain-sensitive areas may become irritated—often felt in the forehead, cheeks, or around the eyes. (Cleveland Clinic; Mayo Clinic)
People often notice it most when they bend forward, lie flat, or wake up congested—positions and timing that can make pressure feel more “concentrated.”
What this guide covers: what a sinus headache is (and what it isn’t) • symptoms and common triggers • home remedies and comfort measures • over-the-counter options to understand (and use carefully) • when it’s worth considering an ENT evaluation at Sleep and Sinus Centers of Georgia
In short: Sinus pressure is common, but true sinus headaches are specific—and the right relief depends on the cause.
What Is a Sinus Headache?
The short definition
A sinus headache generally refers to head or facial pain that occurs alongside sinus inflammation and congestion—often when sinus drainage is blocked. (Cleveland Clinic) In plain terms, it’s not “just a headache.” It’s head/facial pain happening in the context of a nose-and-sinus problem.
How sinus pressure builds (swollen sinus lining + mucus blockage)
When the sinus lining becomes inflamed—due to a cold, allergies, or sinusitis—mucus may thicken and drainage pathways can narrow. The result can be congestion, facial fullness, and the “pressure” sensation many people describe. (Mayo Clinic; Harvard Health)
You might notice the discomfort is more “deep and heavy” than sharp. Some people describe it as wearing a tight mask across the face.
Common misconception: many “sinus headaches” are actually migraines
A key reason sinus headache relief can be frustrating is that many self-diagnosed sinus headaches turn out to be migraine. Migraine can cause facial pressure and even nasal symptoms (like congestion or runny nose), which easily leads to confusion. (WebMD; Cleveland Clinic) If you’ve tried typical sinus fixes repeatedly with limited improvement, it’s worth reconsidering the diagnosis—not because your symptoms aren’t real, but because the cause may be different. In short: If your “sinus headaches” don’t respond to sinus care, consider migraine as a possible driver.
Sinus Headache Symptoms (What You May Notice)
Head/facial pressure symptoms
Common symptoms can include: forehead pressure • pain or fullness around the eyes and cheeks • facial tenderness (especially when bending forward) (Cleveland Clinic; Mayo Clinic)
A practical example: some people feel it most when leaning over to tie shoes, lifting a laundry basket, or doing yoga poses that put the head below the heart.
Congestion and drainage symptoms
A true sinus-related issue often comes with nasal symptoms such as: stuffy nose • thick mucus • postnasal drip (Cleveland Clinic; Mayo Clinic)
Postnasal drip can also contribute to throat irritation or coughing, especially at night, which can further disrupt sleep and make headaches feel worse the next day.
When symptoms suggest infection instead of just inflammation
Some symptoms can signal a larger illness burden—such as fever, significant fatigue, or symptoms that persist or worsen rather than gradually improving. These are reasons many people choose to check in with a clinician rather than treating at home indefinitely. (Mayo Clinic; Cleveland Clinic)
If you’re stuck in a cycle of “a little better, then worse again,” that pattern is also worth discussing with a professional.
In short: Facial pressure plus nasal symptoms point to sinus involvement—persistent fever, thick drainage, or worsening symptoms deserve a closer look.

Causes of Sinus Headaches (And What Triggers Them)
Sinusitis (sinus infection or inflammation)
A sinusitis headache may happen when sinus inflammation follows a cold or upper respiratory infection. Many sinus infections are viral, and symptoms may improve with time and supportive care; bacterial infection is a different scenario and is evaluated differently. (Harvard Health; Mayo Clinic)
Clinicians often emphasize that the timing matters: symptoms that drag on or worsen instead of slowly resolving are a common reason to reassess what’s going on.
Allergies and allergic inflammation
Allergies can inflame nasal tissues, increasing mucus and swelling that blocks drainage. That blockage can contribute to facial pressure and headache-like discomfort—especially during high-pollen seasons or with indoor triggers like dust. (Mayo Clinic; Harvard Health)
If your symptoms seem to show up on repeat—same season, same environment, same exposures—an allergy component becomes more likely.
Barometric pressure or weather changes
Weather shifts don’t “cause” sinus disease by themselves, but changes in barometric pressure may make existing congestion or inflammation feel worse, amplifying pressure sensations. (Houston Methodist)
Some people notice this with storms or big temperature swings—especially if they’re already fighting congestion.
Structural or chronic issues (when headaches keep returning)
If symptoms keep recurring, there may be ongoing inflammation, chronic sinusitis patterns, or nasal obstruction contributing to poor drainage. For a deeper dive, see Sleep and Sinus Centers of Georgia’s guide on sinus head pressure and ENT-related causes: https://sleepandsinuscenters.com/blog/sinus-head-pressure-ent-causes-and-treatments
In short: Triggers vary—colds, allergies, weather, and structural issues can all reduce drainage and ramp up pressure.
Sinus Headache vs Migraine vs Tension Headache (Don’t Treat the Wrong Problem)
Why misdiagnosis is so common
Migraine can overlap with “sinus” symptoms—facial pressure, watery eyes, congestion—so people may assume the sinuses are the problem even when the primary issue is neurologic. (WebMD; Cleveland Clinic) This overlap is one reason you can do “all the sinus things” and still feel stuck.
Clues your “sinus headache” may be a migraine
Symptoms more typical of migraine include: nausea • sensitivity to light or sound • throbbing pain (often one-sided) • feeling worse with activity (WebMD). For more detail, read Migraine vs Sinus Headache: Key Differences and Symptoms Explained: https://sleepandsinuscenters.com/blog/migraine-vs-sinus-headache-key-differences-and-symptoms-explained
When it may be a tension headache
Tension-type headaches are often described as a tight band-like pressure, sometimes associated with stress, jaw clenching, and neck/shoulder tightness. These can be mistaken for sinus pressure because the discomfort may sit across the forehead.
A quick self-check: if your nose feels clear and you’re mainly noticing muscle tightness (neck, jaw, shoulders), tension may be more likely than sinus blockage.
When to ask a clinician for confirmation
If you’re repeatedly treating “sinus headaches” and not improving—or if symptoms follow a migraine-like pattern—confirmation can save time and reduce trial-and-error. (Cleveland Clinic; WebMD)
In short: If your symptoms match migraine or tension patterns, getting the right diagnosis helps you choose the right treatment.
Fast Home Remedies for Sinus Headache Relief (Patient-Friendly Options)
If you’re looking for how to get rid of a sinus headache fast, the most helpful non-prescription strategies generally focus on loosening mucus, supporting drainage, and reducing facial discomfort. (Harvard Health; Cleveland Clinic; Houston Methodist)
Think “open, thin, and drain”: open the passages, thin the mucus, and encourage movement out of the sinuses.
Warm compress for facial pain and pressure
A warm (not hot) compress placed over the cheeks or forehead for about 10–15 minutes may ease facial pain and provide gentle sinus pressure relief. (Harvard Health)
If you’re short on time, many people use this during a morning flare-up or before bed to make resting easier.
Steam inhalation (shower steam or bowl method)
Steam may help moisten nasal passages for some people; effects vary, and you should avoid it if heat or steam worsens symptoms (for example, if you have heat sensitivity or asthma). If using a bowl method, take care to avoid burns and stop if heat worsens irritation. (Harvard Health)
A simple option: sit in the bathroom with a hot shower running for a few minutes and breathe normally—no extreme heat required.
Saline nasal spray (gentle moisture + mucus thinning)
Saline spray can help moisturize and loosen mucus. It’s a simple option many people use during colds or dry winter months. (Cleveland Clinic; Harvard Health)
This can be especially useful if indoor heating dries the air and makes congestion feel “stuck.”
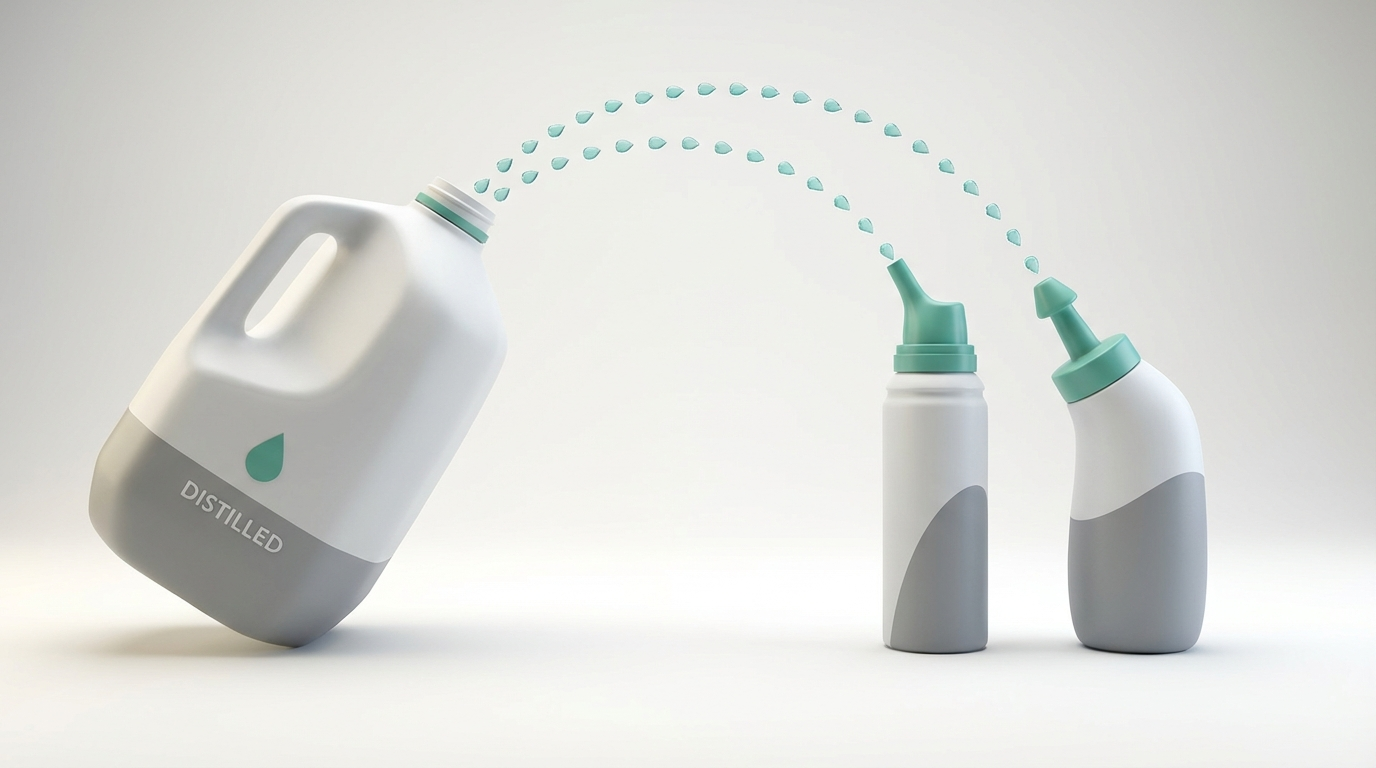
Saline nasal rinses (neti pot/squeeze bottle)
Nasal irrigation can help rinse out mucus and allergens and may improve drainage for some people. Water safety matters: use distilled/sterile water (or previously boiled and cooled) and keep devices clean. Learn more here: https://sleepandsinuscenters.com/blog/neti-pot-water-safety-why-boiled-or-distilled-water-is-essential-a906d (Harvard Health; Cleveland Clinic)
If you’re new to rinses, start gently and follow device directions—comfort and technique make a big difference.
Hydration
Drinking enough fluids can support thinner mucus and easier drainage. Warm beverages may also feel soothing when congestion is prominent. (Harvard Health)
If you’re not drinking much because you feel run-down, setting a simple goal (like a glass of water with each meal) can help.
Elevate your head when resting/sleeping
Sleeping with the head slightly elevated may reduce pooling and help drainage, which can contribute to sinus headache relief overnight. (Harvard Health)
A small extra pillow or a slight bed incline is often enough—no complicated setup needed.
Simple environment tweaks
Humidifier: adding moisture may reduce dryness and irritation—keep it clean. • Avoid smoke/strong fragrances: these can worsen nasal irritation and swelling. (Houston Methodist; Harvard Health) If you prefer non-medication approaches, you may also like Managing Sinus Headaches Without Pills: https://sleepandsinuscenters.com/blog/managing-sinus-headaches-without-pills
In short: Warmth, moisture, saline, hydration, and head elevation are low-risk basics that often help pressure move and pain ease.

Over-the-Counter Treatments (What Helps and What to Use Carefully)
OTC options for sinus headache treatment generally fall into two categories: pain control and congestion/inflammation control. Always follow label directions and consider checking with a clinician or pharmacist if you have chronic conditions or take other medications. (Mayo Clinic; Cleveland Clinic; Harvard Health)
A pharmacist-style way to think about it: treat the “pressure system” (inflammation/congestion) and the pain signal (headache).
Pain relievers for headache pain
Acetaminophen or NSAIDs (like ibuprofen/naproxen) are commonly used for headache pain. Each has label precautions and may not be ideal for everyone (for example, certain stomach, kidney, bleeding, or liver concerns). (Mayo Clinic)
If you’re unsure what’s safest with your medical history, ask before stacking products—especially combination cold/flu meds that may include similar ingredients.
Decongestants (short-term relief)
Oral decongestants may reduce congestion but can be a concern for some people with high blood pressure or certain heart conditions. Nasal decongestant sprays can feel very effective short-term, but overuse can lead to rebound congestion. If this is a concern for you, see more on rebound congestion risk: https://sleepandsinuscenters.com/blog/afrin-rebound-how-long-does-nasal-congestion-last-after-use (Mayo Clinic; Harvard Health)
If you feel like you “can’t breathe without it,” that’s a sign to pause and get guidance.
Antihistamines (if allergies are part of the problem)
Antihistamines may help if allergic symptoms are driving congestion. Some are sedating while others are less likely to cause drowsiness—an important practical difference for daytime use. (Mayo Clinic)
If your symptoms are seasonal or exposure-related, antihistamines may fit more logically than decongestants alone.
Nasal steroid sprays (for inflammation control)
Intranasal steroid sprays help reduce inflammation and are often most useful when taken consistently, especially for allergy-related swelling. They don’t typically provide instant relief, but can improve symptoms over time. (Mayo Clinic; Harvard Health)
Many people do best when they treat these sprays like “daily maintenance,” not a one-time rescue.
Combination approach (a realistic “at-home plan”)
A common, practical approach for sinus headache relief may look like: saline rinse or spray for mucus/drying • a nasal steroid spray for inflammation (if appropriate) • a pain reliever as needed for discomfort. This type of plan targets both congestion and pain, which is often necessary when pressure and headache overlap. (Harvard Health; Mayo Clinic)
In short: Match treatment to the problem—combine careful pain control with strategies that reduce swelling and help sinuses drain.
Medical Treatments (When Home Care Isn’t Enough)
When antibiotics might be considered (and when they aren’t)
Because many sinus infections are viral, antibiotics aren’t always the right tool. Persistent, worsening, or complicated symptoms are often reasons clinicians evaluate whether bacterial infection is more likely. (Harvard Health; Mayo Clinic; Cleveland Clinic)
If you’re hoping for a “quick fix,” it helps to know that the best treatment depends on the cause—not just the discomfort level.
Prescription nasal sprays or stronger anti-inflammatory treatment
In some cases, prescription therapies may be used to better control inflammation, improve nasal airflow, and reduce recurrence. (Mayo Clinic)
Allergy evaluation and treatment plans
If headaches and congestion track with seasons, pets, or indoor exposures, allergy testing and a long-term control plan may reduce flare-ups. (Harvard Health; Mayo Clinic)
When an ENT evaluation can help
An ENT visit can be helpful for persistent or recurrent symptoms, suspected structural blockage, or chronic sinusitis patterns. If you’re looking for next steps, Sleep and Sinus Centers of Georgia can help evaluate ongoing sinus pressure and recurring symptoms. This article mentions Sleep and Sinus Centers of Georgia as a local resource example; many other qualified providers also offer comprehensive ENT care.
In short: If symptoms are severe, persistent, or recurring, medical evaluation can clarify the cause and open the door to targeted treatment.

When to See a Doctor (Red Flags You Shouldn’t Ignore)
Seek care urgently if you have
Severe headache with high fever • swelling around the eyes or vision changes • stiff neck, confusion, or neurologic symptoms (Mayo Clinic; Cleveland Clinic)
Make an appointment if
Symptoms last more than 7–10 days or worsen after initial improvement • you have recurrent “sinus headaches” (migraine or chronic sinusitis may be involved) • you rely on decongestant sprays frequently (Mayo Clinic; Cleveland Clinic)
In short: Don’t wait on red flags or a pattern of recurring symptoms—prompt evaluation helps prevent complications and misdiagnosis.
Lifestyle Tips to Prevent Sinus Headaches
Prevent colds and infection triggers
Handwashing, adequate sleep, and hydration support overall resilience during cold/flu season. (Cleveland Clinic)
Allergy control basics
Reducing exposure to dust/pollen and addressing indoor air quality can help limit swelling that contributes to blockage. (Houston Methodist)
Keep sinuses draining well
Some people use saline spray/rinses during high-risk seasons to reduce mucus buildup and irritant exposure (as tolerated and with safe water practices). (Harvard Health)
Track patterns
A simple symptom log (weather shifts, seasonal timing, foods, stress, sleep changes) can help clarify whether episodes fit sinusitis patterns or look more like migraine triggers.
In short: Healthy routines, allergy control, and proactive saline care can reduce flare-ups and keep drainage pathways moving.
FAQs About Sinus Headache Relief
How do I get rid of a sinus headache fast?
The quickest comfort strategies tend to be warmth (compress), moisture (steam/shower), saline spray/rinse, hydration, and rest with head elevation—especially when congestion is prominent. (Harvard Health; Houston Methodist)
Is it safe to use a decongestant spray every day?
Many sources warn that overusing topical decongestant sprays can cause rebound congestion, which can prolong symptoms and create a cycle of dependence. (Mayo Clinic)
Can a sinus headache actually be a migraine?
Yes. Migraine can cause facial pressure and nasal symptoms, which is why mislabeling is common. (WebMD; Cleveland Clinic)
Do warm compresses and steam really work?
They may help by soothing facial discomfort and moistening irritated nasal passages. Effects vary by person and by the underlying cause. (Harvard Health)
When should I suspect a sinus infection?
Fever, thick nasal drainage, and symptoms that persist or worsen instead of gradually improving can be reasons to seek evaluation. (Mayo Clinic; Cleveland Clinic)
Conclusion — A Simple Plan for Relief + Next Steps
For many people, sinus headache relief comes down to three goals: reduce inflammation, relieve congestion, and promote drainage. Start with patient-friendly basics like saline, moisture, warmth, hydration, and smart OTC choices when appropriate. If symptoms keep returning, it may be time to consider whether migraine, allergies, or chronic sinusitis is the real driver.
If you’d like help sorting out recurring symptoms or ongoing pressure, book an appointment with Sleep and Sinus Centers of Georgia to discuss next steps: https://www.sleepandsinuscenters.com/
Sources
Cleveland Clinic — Sinus Headaches: https://my.clevelandclinic.org/health/diseases/9641-sinus-headaches
Harvard Health — How to get rid of a sinus headache: https://www.health.harvard.edu/diseases-and-conditions/how-to-get-rid-of-a-sinus-headache
Mayo Clinic — Sinus headaches (diagnosis & treatment): https://www.mayoclinic.org/diseases-conditions/sinus-headaches/diagnosis-treatment/drc-20377584
Houston Methodist — Fastest way to get sinus pressure relief: https://www.houstonmethodist.org/blog/articles/2024/feb/whats-the-fastest-way-to-get-sinus-pressure-relief/
WebMD — Sinus Headaches vs Migraine: https://www.webmd.com/migraines-headaches/sinus-headaches
This article is for educational purposes only and is not medical advice. Please consult a qualified healthcare provider for diagnosis and treatment.
Don’t let allergies slow you down. Schedule a comprehensive ENT and allergy evaluation at Sleep and Sinus Centers of Georgia. We’re here to find your triggers and guide you toward lasting relief.








