Radiofrequency Turbinate Reduction vs Turbinoplasty: Which Is Better for Nasal Congestion?
If you’re stuck in the cycle of sprays, allergy meds, and “still can’t breathe,” your turbinates may be part of the reason. This guide compares radiofrequency turbinate reduction vs turbinate surgery (often called turbinoplasty) in a patient-friendly way—covering effectiveness, recovery, risks, candidacy, and long-term outcomes—so you can understand the options and ask better questions at your ENT visit.
Medical disclaimer: This article is for education only and isn’t a substitute for individualized medical evaluation or treatment.
What are turbinates—and why do they cause nasal congestion?
Inside your nose are structures called turbinates (inferior, middle, and superior). A helpful way to picture them: they’re like the “air-conditioning fins” of the nose—conditioning incoming air before it reaches the lungs. When they swell or become chronically enlarged, airflow narrows and breathing can feel restricted even though your nose looks normal from the outside. For a plain-language overview, see Cleveland Clinic’s explanation of turbinate reduction.
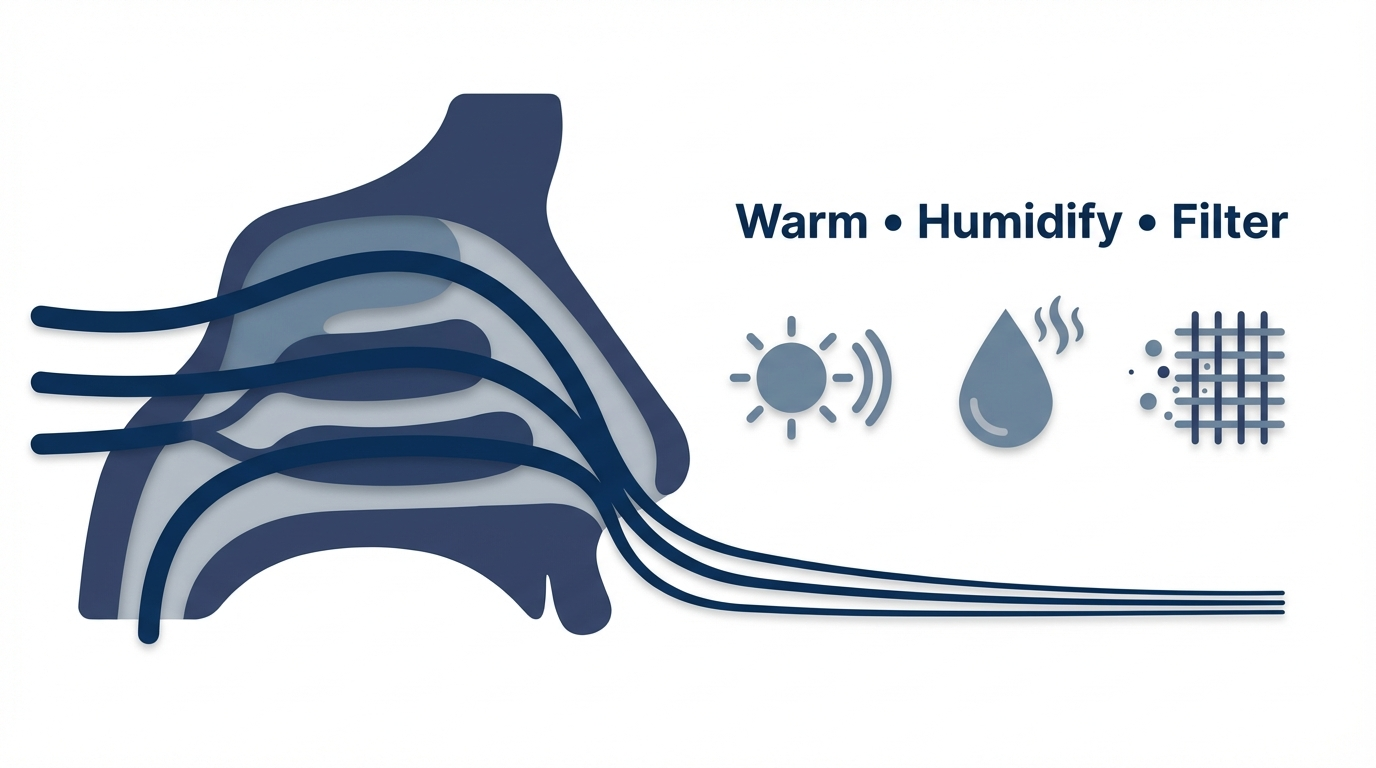
What turbinates do (and why you want them)
Turbinates help:
- Warm and humidify inhaled air
- Filter particles and irritants
- Support smooth airflow patterns
Because they are functional, “more open” is not always better. Modern turbinate reduction techniques aim to improve airflow while preserving function—an important concept when discussing rare complications like empty nose syndrome.

What is turbinate hypertrophy?
Turbinate hypertrophy means the turbinate tissue is chronically swollen or enlarged, narrowing the nasal airway and contributing to nasal obstruction. Symptoms often fluctuate—worse at night, during allergy seasons, or in dry air—because the nasal lining responds to inflammation and environmental triggers.
For a deeper overview, see our guide on turbinate reduction.
- In short: healthy turbinates matter; the goal is right-sized, functional airflow, not “as much removal as possible.”
Symptoms: how to tell if your turbinates might be the problem
Common symptoms of enlarged turbinates
People with turbinate-related blockage often report:
- Ongoing nasal congestion or “stuffy nose”
- Mouth breathing and dry mouth (especially overnight)
- Poor sleep, snoring, or daytime fatigue
- Sometimes a reduced sense of smell
- Post-nasal drip or pressure (varies by person)
Real-life example: Some patients breathe better after a hot shower but feel blocked again later. That pattern often points to inflammation-driven swelling rather than a fixed obstruction alone.
Signs it may be more than turbinates
Other contributors can include:
- Deviated septum (often more one-sided blockage). Learn more about deviated septum relief.
- Nasal polyps or chronic sinus inflammation
- Rebound congestion from frequent decongestant spray use (Afrin-type products)
A helpful clue clinicians listen for: if one side consistently feels tighter, a septal deviation or nasal valve issue may be part of the story—not just turbinate swelling.
- In short: symptoms can overlap; a focused exam helps distinguish swelling from structural blockage.
Causes of turbinate enlargement (why it keeps coming back)
Inflammation-related causes
Common drivers include:
- Allergic rhinitis (seasonal or year-round)
- Non-allergic rhinitis (irritants, weather changes, fragrances)
- Chronic sinus or nasal lining inflammation
If your symptoms spike with pollen, indoor dust, strong scents, or abrupt temperature changes, inflammatory swelling is likely part of the picture—one reason ongoing medical management may still be helpful, even after a procedure.
Structural and lifestyle contributors
These can worsen symptoms or make blockage harder to control:
- Deviated septum that changes airflow patterns
- Dry environments, smoke exposure, and airborne irritants
- A “sleep-disruption loop,” where poor sleep amplifies inflammation and sensitivity
Think of it like a narrow hallway: if the septum shifts the wall inward and turbinates swell at the same time, the passage can feel dramatically tighter—even if each issue alone seems mild.
- In short: inflammation, anatomy, and environment interact; lasting relief often requires addressing more than one factor.
Treatment pathway before surgery (what ENTs usually try first)
Medical treatments
Before procedures, ENTs commonly recommend steps such as:
- Saline rinses and moisture strategies
- Intranasal steroid sprays (technique matters)
- Antihistamines and allergy management strategies
- Addressing overuse of topical decongestant sprays if relevant
Small technique changes can make medical therapy work better. For example, aiming a nasal steroid slightly outward (toward the ear on the same side) often reduces irritation and helps medication reach the areas that swell.
When “maximal medical therapy” isn’t enough
Procedures are discussed when nasal blockage continues to impact sleep or quality of life and turbinate hypertrophy is confirmed on exam (sometimes with nasal endoscopy). Cleveland Clinic provides more details on when turbinate reduction is considered.
A practical summary you might hear: “If you’ve done the right meds the right way and the tissue is still physically in the way, reducing the tissue may help.”
- In short: try targeted medical therapy first; procedures are for persistent, exam-proven blockage.

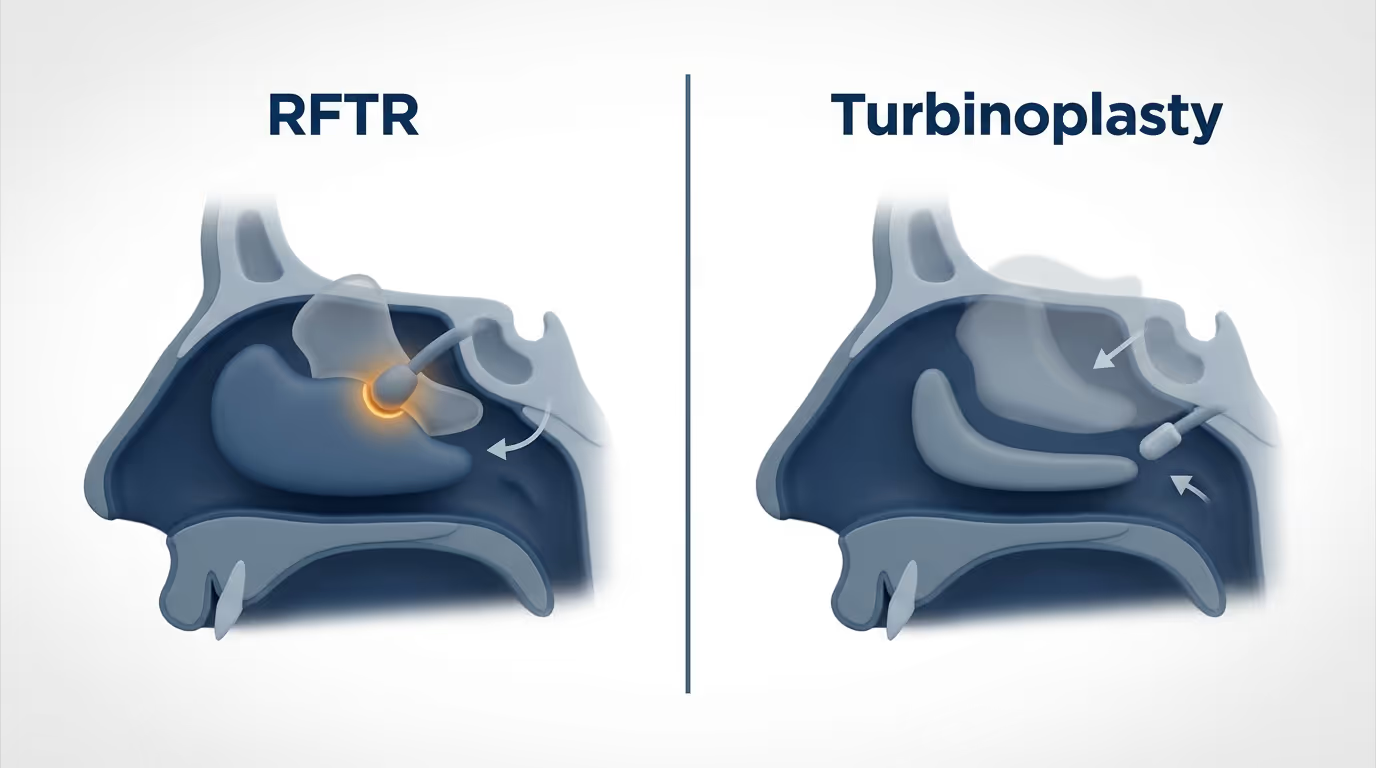
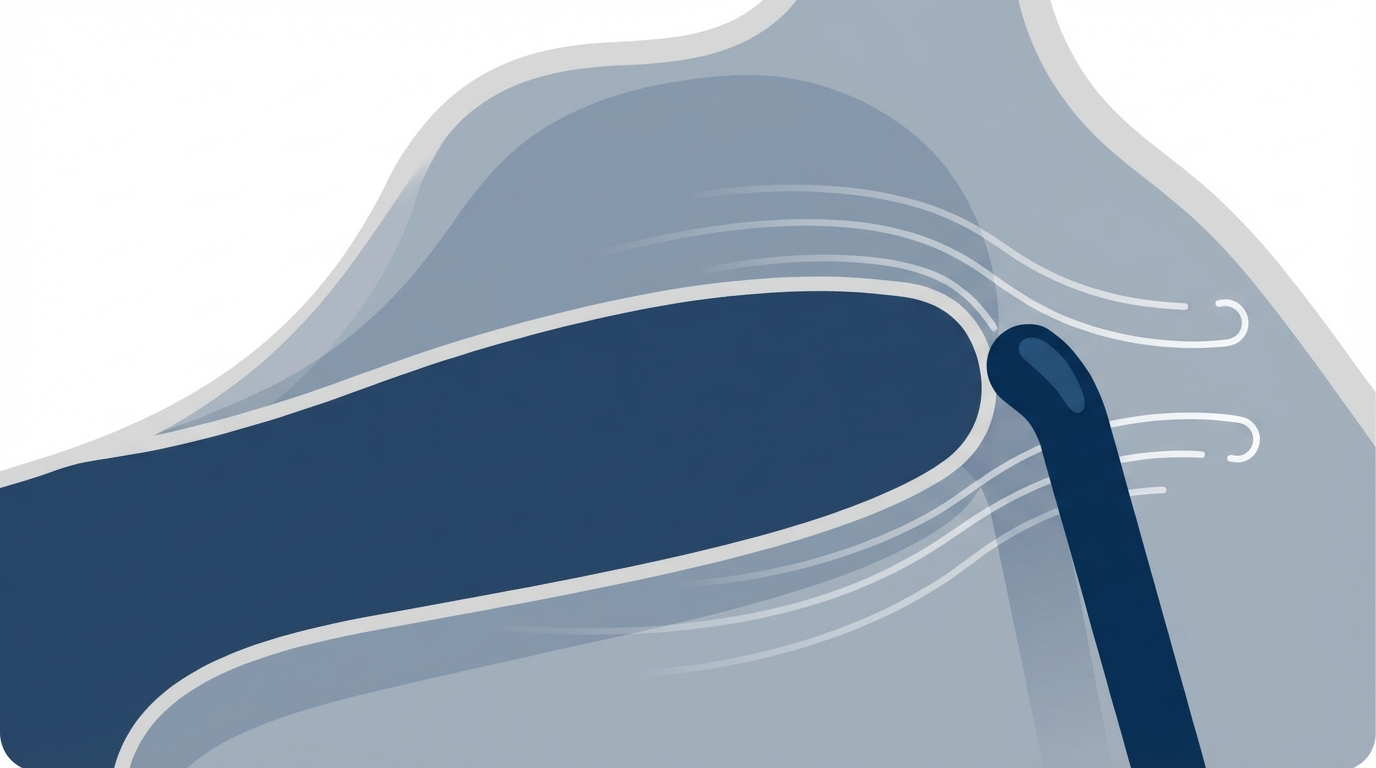
Radiofrequency turbinate reduction (RFTR): what it is and how it works
What RFTR actually does
Radiofrequency turbinate reduction uses controlled energy to shrink turbinate tissue from within. Rather than cutting away large areas of lining, it reduces volume while keeping the surface tissue as intact as possible—a function-preserving approach. See ENT & Audiology News and Cleveland Clinic for overviews.
A helpful analogy: RFTR is more like “deflating” the tissue than “removing” it. Studies and patient reports suggest it’s often associated with less crusting and a smoother early recovery than more invasive methods.
How the procedure is typically done
RFTR is commonly performed in an outpatient setting, frequently under local anesthesia. In general, it involves:
- Minimal cutting
- Typically less bleeding and less crusting than more invasive approaches
- Often little to no nasal packing
To learn more, see our article on radiofrequency ablation for nasal obstruction.
- In short: RFTR is a minimally invasive, function-preserving approach designed to reduce volume with a relatively easy recovery.
Turbinate surgery (turbinoplasty): what it is and how it works
What “turbinate surgery” can mean
“Turbinate surgery” is a broad term and may refer to:
- Turbinoplasty (reshaping/reducing while preserving the lining when possible)
- Submucosal reduction (reducing tissue beneath the lining)
- Turbinectomy (removing more turbinate tissue—now generally used cautiously)
Technique matters, and surgeons may use different combinations depending on anatomy and goals. The AAO-HNS/F clinical consensus provides more context for these approaches.
How traditional turbinoplasty is typically performed
Compared with RFTR, turbinoplasty often involves more direct tissue removal or repositioning. It may:
- Have more postoperative crusting or bleeding (depending on technique and extent)
- More commonly involve packing (surgeon-dependent)
- Be performed in an operating room—especially if combined with septoplasty or sinus surgery
Common scenario: If you’re already planning septoplasty or sinus surgery, your surgeon may recommend addressing turbinates in the same setting to improve airflow “from both sides”—structure (septum) and soft tissue (turbinates).
- In short: turbinoplasty offers stronger reshaping when needed, with a typically more involved recovery.
Radiofrequency turbinate reduction vs turbinoplasty: practical comparison
Here’s a concise, patient-centered comparison of what most people ask about—downtime, comfort, and results:
- Invasiveness and setting
- RFTR: Minimally invasive; commonly outpatient/local anesthesia
- Turbinoplasty: Often more invasive; frequently done in the OR, especially when combined with septoplasty or sinus surgery
- Bleeding and crusting
- RFTR: Typically less
- Turbinoplasty: Can be more, depending on technique and extent
- Nasal packing
- RFTR: Often minimal or none
- Turbinoplasty: More likely in some cases (surgeon-dependent)
- Recovery and aftercare
- RFTR: Generally faster recovery; simpler aftercare
- Turbinoplasty: Recovery may be longer; follow-up cleaning/debridement may be needed
- Effectiveness for nasal obstruction
- Both improve symptoms for many people. Some comparative studies suggest turbinoplasty may have a small long-term edge, though results are not consistently or significantly better across all research.
- Durability
- RFTR: Can be durable, but symptoms may recur if underlying inflammation persists
- Turbinoplasty: Often durable, but outcomes still depend on ongoing inflammation control and surgical technique
What the research suggests
Both options can help nasal obstruction. Systematic reviews and comparative studies (PubMed; PMC; ENT & Audiology News) indicate that while turbinoplasty sometimes shows modest long-term advantages, findings vary by study and patient selection.
- In short: there’s no one-size-fits-all “winner”—the right choice depends on your anatomy, inflammation, goals, and tolerance for recovery time.
Risks and complications (for both options)
Common short-term effects
- Temporary swelling and “worse-before-better” congestion
- Mild bleeding
- Crusting during healing (often less with RFTR)
Less common but important risks
- Chronic dryness
- Ongoing or recurrent nosebleeds
- Infection (uncommon)
Empty nose syndrome (ENS): what to know
Empty nose syndrome is a rare but important complication where someone may feel obstructed even if nasal passages look open. It’s more associated with aggressive turbinate removal, which is one reason conservative, function-preserving approaches are emphasized today. For a patient-focused overview, see our article on empty nose syndrome. With contemporary conservative techniques, ENS is considered very rare.
- In short: most side effects are temporary; serious complications are uncommon, and modern techniques aim to preserve function.
Who is a better candidate for RFTR vs traditional surgery?
RFTR may be a good fit if you:
- Prefer a minimally invasive option
- Have turbinate hypertrophy without significant structural blockage
- Want shorter downtime and simpler aftercare
Turbinoplasty may be considered if you:
- Have more significant turbinate enlargement requiring stronger reduction
- Are already having septoplasty or sinus surgery (combined approach)
- Need more structural reshaping (technique-dependent)
The “hidden factors”: septum, nasal valves, and allergies
A complete evaluation matters because treating only one piece of the puzzle can leave symptoms behind. Turbinates, the septum, nasal valves, and inflammation can all contribute to nasal obstruction—and the best plan depends on which factor is dominant. Learn more about deviated septum relief and see our turbinate reduction overview for context.
- In short: the best results come from targeting the right problem—soft tissue, structure, inflammation, or a combination.

What recovery looks like (patient-friendly timeline)
RFTR recovery basics
- A few days of tenderness, swelling, and congestion are common
- Breathing typically improves gradually as swelling resolves
- Saline rinses/sprays and humidification can reduce dryness and crusting
Practical tip: It’s common to feel “more open” in week two than week one, even if day three felt discouraging. Recovery is typically gradual rather than instant.
Turbinoplasty recovery basics
- Early congestion is expected (sometimes longer-lasting than with RFTR)
- More crusting is common and requires careful aftercare
- Follow-ups may include cleaning/debridement (technique-dependent)
- Temporary activity restrictions help reduce bleeding risk
For many patients weighing radiofrequency turbinate reduction vs turbinoplasty, recovery time and aftercare are key deciding factors—especially when work and sleep are already impacted.
- In short: RFTR often offers a gentler recovery; turbinoplasty can be more involved but may be preferred when stronger reshaping is needed.
Lifestyle tips to reduce nasal congestion (before and after a procedure)
Humidity and nasal moisture
- Use a humidifier appropriately (avoid over-humidifying)
- Keep a consistent saline spray or rinse routine if it agrees with you
Allergy and irritant control
- Minimize dust/pollen exposure when possible
- Avoid smoke and strong fragrances that can trigger swelling
Sleep-focused tips
- Consider elevating the head of the bed
- Address mouth breathing and comfort issues that can worsen poor sleep patterns
- In short: daily habits and environment can meaningfully reduce congestion and help maintain procedure results.
FAQs
Is radiofrequency turbinate reduction painful?
Most people describe RFTR as pressure and soreness rather than sharp pain when local anesthesia is used. Experiences vary by individual and technique.
How long does RFTR last?
RFTR can provide long-lasting improvement for some people, but symptoms can return if underlying inflammation (allergies/rhinitis) remains active.
Is turbinate surgery permanent?
Turbinoplasty can create a more structural change, but turbinates can still swell with allergies or irritation over time.
Which one has faster recovery: RFTR or turbinoplasty?
In many cases, RFTR has quicker recovery and less crusting than more invasive turbinoplasty techniques, as described by Cleveland Clinic.
Can turbinate reduction help snoring or sleep apnea symptoms?
Improving nasal airflow may reduce mouth breathing and improve sleep comfort for some people. Sleep apnea is multifactorial, so nasal procedures are often just one part of a broader plan.
What are signs turbinate reduction “didn’t work”?
Persistent nasal obstruction after the expected healing window may suggest ongoing inflammation, another structural issue (like the septum or nasal valves), or that the reduction was insufficient.
Can turbinates enlarge again after either procedure?
Yes. Turbinates can swell again due to inflammation or triggers—even after reduction—especially if allergic or non-allergic rhinitis isn’t well controlled.
Is empty nose syndrome common?
ENS is considered rare, and the risk is lower with conservative, function-preserving techniques. See our ENS overview for details.
- In short: both procedures can help; success depends on your anatomy, inflammation control, and proper aftercare.
Conclusion: which is better for nasal congestion?
When weighing radiofrequency turbinate reduction vs turbinoplasty, the “better” option depends on your anatomy, symptom severity, and whether inflammation or structural blockage is driving the problem.
- RFTR is often preferred for being minimally invasive, typically easier to recover from, and function-preserving.
- Turbinoplasty can be equally effective and, in some studies, may show a modest long-term edge for obstruction relief—though findings are mixed and not consistently significant across all research (see PubMed, PMC, and ENT & Audiology News).
At Sleep and Sinus Centers of Georgia, an individualized evaluation can clarify whether turbinates, the septum, nasal valves, allergies—or a combination—are contributing to your symptoms. No single approach is right for everyone, and no outcomes are guaranteed, but a tailored plan can maximize the chances of meaningful relief.
If you’re dealing with chronic nasal congestion or suspected turbinate hypertrophy, schedule an evaluation with Sleep and Sinus Centers of Georgia to review your exam findings and discuss options. You can book an appointment here.
This article is for educational purposes only and is not medical advice. Please consult a qualified healthcare provider for diagnosis and treatment.
Don’t let allergies slow you down. Schedule a comprehensive ENT and allergy evaluation at Sleep and Sinus Centers of Georgia. We’re here to find your triggers and guide you toward lasting relief.