Oral Appliance for Sleep Apnea: Does It Really Work?
If you’ve been diagnosed with obstructive sleep apnea (OSA)—or you suspect you might have it—you may be wondering whether a less bulky option than CPAP could still make a real difference. An oral appliance for sleep apnea is one of the most common alternatives, and for the right person, it can be a highly effective treatment.
Below is a clear, research-based look at how oral appliances work, who they help most, how they compare with CPAP, what side effects to watch for, and what the next steps usually look like.
Quick Answer: Do Oral Appliances Really Work for Sleep Apnea?
The short version
Yes—oral appliances can be highly effective for obstructive sleep apnea, particularly mild to moderate cases. Research commonly finds that around 70% of patients have meaningful improvement and about one-third may see near-complete symptom resolution, while roughly one-third may have little improvement—so follow-up testing is essential. Effectiveness varies by severity, airway anatomy, and how consistently the device is used. [1][3][4]
Why they’re often “as effective” as CPAP in real life
CPAP is typically more powerful at reducing breathing events when it’s worn. Many people, however, use oral appliances more consistently (more nights per week and more hours per night). That higher adherence can narrow the real-world outcome gap—so for many patients, the “best” therapy is the one they can actually use consistently. [2][3][4] Oral appliance therapy typically requires nightly, ongoing use to maintain its benefits.
Bottom line: In real life, the most effective therapy is the one you can stick with and verify on follow-up testing.
What Is an Oral Appliance for Sleep Apnea?
Definition (patient-friendly)
An oral appliance is a small device worn while sleeping that helps keep your airway open—essentially a custom-fit mouthpiece designed to reduce airway collapse during sleep. [1][2] If CPAP is like “air splinting” your airway open, an oral appliance gently changes jaw and tongue position so the airway is less likely to pinch closed in the first place.
The two main types
- Mandibular advancement device (MAD): The most common option. It gently guides the lower jaw forward to help keep the airway from narrowing. [1][2]
- Tongue-retaining device (TRD): Holds the tongue forward to reduce blockage; used less often than MADs. [1][2]
Custom-made vs over-the-counter “boil-and-bite”
Over-the-counter mouthguards may fit poorly and don’t allow precise adjustment. Sleep medicine and dental sleep specialists generally recommend custom-fitted, clinician-directed oral appliance therapy for better comfort, safety, and effectiveness—especially when treating a diagnosed medical condition like OSA. [2][4] A boil-and-bite guard might feel “fine” at first, but if it can’t be titrated (incrementally adjusted), you lose one of the most important parts of therapy—dialing in the smallest jaw advancement that still delivers meaningful improvement.
Bottom line: Custom, adjustable devices directed by a trained clinician are more likely to be safe, comfortable, and effective than over-the-counter options.

OSA Basics—Symptoms and Why Treatment Matters
Common symptoms of obstructive sleep apnea
- Loud snoring (but not always)
- Gasping or choking during sleep
- Witnessed breathing pauses
- Morning headaches or dry mouth
- Daytime sleepiness, low energy, brain fog
- Mood changes or irritability
It’s also possible to have OSA without obvious snoring, so testing matters if symptoms or risk factors are present.
Health risks of untreated OSA
- High blood pressure and cardiovascular strain
- Daytime driving and workplace safety issues due to sleepiness
- Reduced quality of life and impaired concentration
Even “mild” sleep apnea can be disruptive if it fragments sleep night after night.
Bottom line: If symptoms or risks are present, testing and timely treatment can protect daily function and long-term health.
How Oral Appliances Work (The “Mechanism” Without the Jargon)
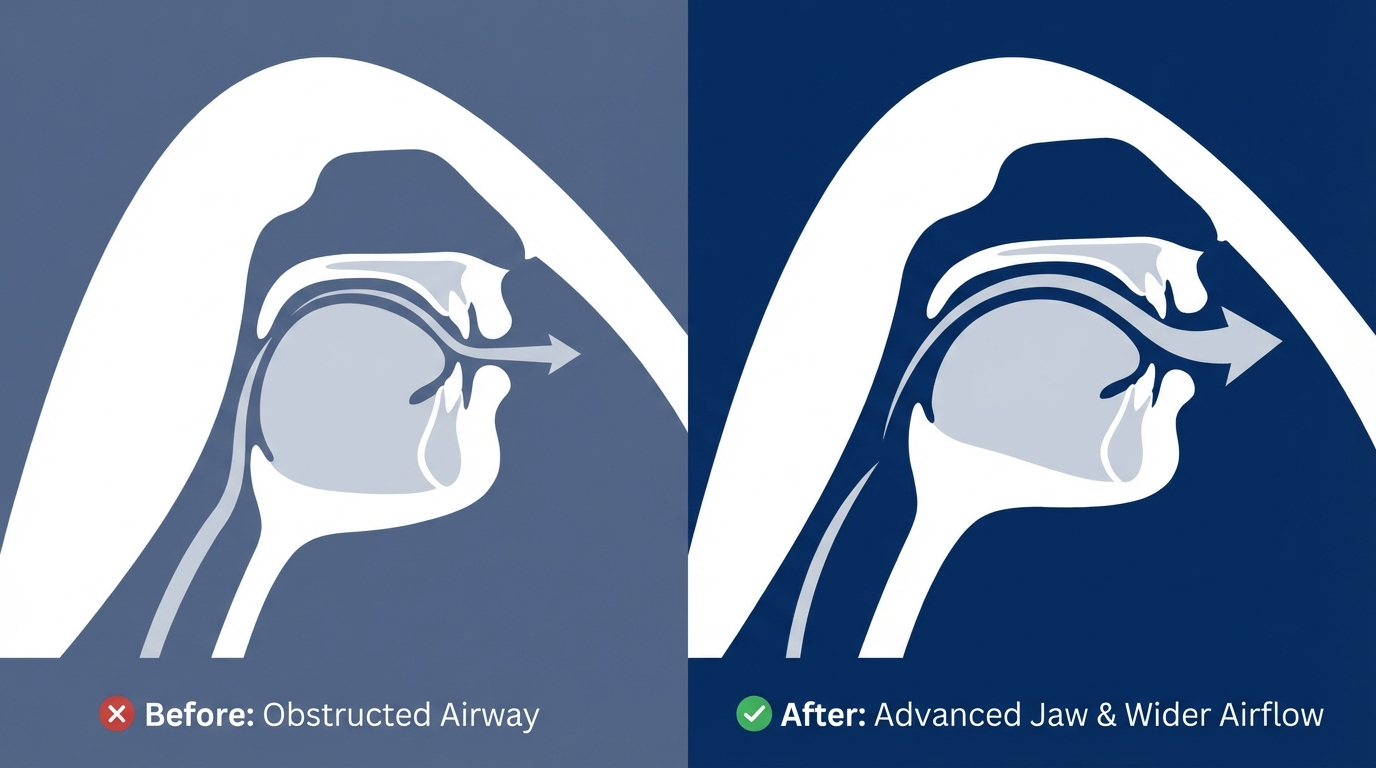
What happens to the airway during sleep
During sleep, throat muscles relax. In OSA, the airway can narrow or collapse repeatedly, reducing airflow and disrupting sleep—like a soft garden hose that kinks more easily when the walls relax.
How a MAD helps
A MAD repositions the lower jaw slightly forward, creating more space behind the tongue and reducing the tendency of soft tissues to collapse into the airway. [1][2] The goal is to find a comfortable advancement that improves breathing without causing jaw strain.
Why this helps snoring too
Snoring often happens when airflow becomes turbulent through a partially narrowed airway. By improving airflow, oral appliances often reduce snoring—though not all snoring is caused by sleep apnea, and quieter snoring doesn’t automatically mean OSA is fully controlled.
Bottom line: Gentle jaw or tongue repositioning can stabilize the airway and often quiet snoring, but effectiveness should be confirmed with objective testing.
Effectiveness: What the Research Says (and What It Means for You)
Real-world success rates
Across studies, oral appliance therapy shows:
- Around 70% of patients: meaningful reduction in OSA severity
- About one-third: near-complete response
- About one-third: minimal change, highlighting the need for objective follow-up testing [1][3][4]
These averages vary by severity, airway anatomy, and adherence.
Mild vs moderate vs severe sleep apnea
Oral appliances are typically recommended as a strong option (often first-line) for mild to moderate OSA. [1][2] If you’re not sure where you fall, understanding your sleep apnea severity (AHI) can help you set expectations. Related: AHI score explained: https://sleepandsinuscenters.com/blog/ahi-score-explained-understanding-your-sleep-apnea-severity
For severe OSA, an oral appliance may still be used—especially if CPAP isn’t tolerated—but it usually requires careful follow-up, realistic targets, and sometimes combination strategies. [1][3][4]
What “works” should mean (beyond fewer events)
- Better daytime alertness and energy
- Reduced snoring (often noted by bed partners)
- Improved sleep quality
- Better objective sleep test results (AHI and oxygen levels)
Bottom line: Treat, then test—symptom relief is great, but objective sleep testing confirms control.

Oral Appliance vs CPAP: Which Is Better?
CPAP—why it’s considered the gold standard
CPAP is widely considered the gold standard because it can be extremely effective at preventing airway collapse when used consistently. [2][3] For very severe OSA or significant oxygen drops, CPAP’s “power” matters.
Oral appliances—why many patients prefer them
- Small and quiet
- Easy to travel with
- Often easier to use nightly (no mask, hose, or machine) [1][2]
For a deeper side-by-side breakdown, see Oral Appliance vs CPAP: https://sleepandsinuscenters.com/blog/oral-appliance-vs-cpap-which-is-right-for-you
The adherence factor
Even though CPAP may outperform oral appliances “on paper,” real-world outcomes can be similar for many patients because oral appliance adherence is often higher. [3][4]
Who might do better with each
- CPAP may be favored when OSA is very severe, oxygen drops are significant, or medical complexity is higher.
- Oral appliances may be favored for mild–moderate OSA, CPAP intolerance, frequent travelers, or patients who prioritize comfort and simplicity (which can improve consistency). Your healthcare provider will consider multiple factors to customize treatment.
Bottom line: Choose the therapy you can use reliably—and verify effectiveness with follow-up testing.
Who Is a Good Candidate for an Oral Appliance?
Strong candidates
- People with mild to moderate OSA
- People who cannot tolerate CPAP due to discomfort, claustrophobia, dryness, or frequent removal during sleep [1][2]
Factors that can affect success
- Jaw and tongue anatomy
- Sleeping position (back vs side)
- Weight changes over time
- Nasal congestion or blockage
- Alcohol use close to bedtime
Who needs extra caution
An oral appliance can still be possible for some patients, but evaluation is especially important if there are:
- Significant TMJ concerns
- Poor dentition, missing teeth, or gum disease
- Severe bite or jaw alignment issues [2]
Bottom line: A candidacy evaluation looks at your airway and your dental/jaw health to match you with the safest, most effective plan.

What to Expect: Fitting, Adjustment, and Follow-Up
Step 1 — Confirm diagnosis
Snoring alone isn’t the same as sleep apnea. A sleep study (home or in-lab) helps confirm OSA and guides appropriate treatment.
Step 2 — Custom fitting and titration
A custom device is made to fit your teeth and bite. Then it’s gradually adjusted (“titrated”) to balance comfort and effectiveness. [2]
Step 3 — Re-testing to confirm it’s working
Because not everyone responds, repeat sleep testing is used to verify that therapy is controlling OSA—not just reducing snoring. [1][3] This step matters even if you feel better.
Ongoing care
Periodic visits help monitor fit, device wear, dental and TMJ health, and bite changes over time. [2]
Bottom line: Expect a process—fit, adjust, then test—to ensure your device is truly working for you.

Side Effects, Risks, and How to Manage Them
Common short-term side effects
Common early effects can include jaw or tooth soreness, dry mouth or increased salivation, and gum irritation. [2][4] Learn more: Oral appliance side effects and management strategies: https://sleepandsinuscenters.com/blog/oral-appliance-side-effects-what-to-expect-and-how-to-manage-them
Potential longer-term issues
Some patients develop bite changes or tooth movement over time, which is why regular monitoring matters. [2] It’s not a reason to avoid therapy—but it is a reason to choose a provider who takes follow-up seriously.
Tips to reduce side effects
- Gradual titration rather than big jumps in advancement
- Morning jaw movement routines (when recommended)
- Routine follow-ups for adjustments and fit checks [2]
Bottom line: Most side effects are manageable with gradual adjustments and regular dental-sleep follow-up.
Lifestyle Tips That Make Oral Appliance Therapy Work Better
Sleep position strategies
Some people experience fewer airway events when sleeping on their side. Positional strategies may be discussed alongside oral appliance therapy.
Weight management (if applicable)
Weight changes can affect airway size and OSA severity, which may change treatment needs over time.
Alcohol and sedatives
Alcohol and certain sedatives can worsen airway collapse for some people, especially close to bedtime.
Nasal breathing support
Managing allergies or nasal obstruction may improve comfort and sleep quality and can support overall adherence.
Bottom line: Small lifestyle adjustments can boost the effectiveness and comfort of your oral appliance.
Costs and Insurance (What Patients Commonly Ask)
What affects total cost
- Custom fabrication
- Visits for fitting and adjustment
- Follow-up sleep testing
- Repairs or replacement over time
For a detailed cost breakdown, see: Mandibular advancement device cost: https://sleepandsinuscenters.com/blog/mandibular-advancement-device-cost-what-to-expect
Does insurance cover it?
Many plans cover oral appliance therapy for diagnosed OSA, but coverage varies. Documentation requirements often include a sleep study and medical necessity; your clinic can help clarify typical insurer requests.
Bottom line: Check your benefits early—coverage often requires a documented diagnosis and medical necessity.
FAQs
Can an oral appliance cure sleep apnea?
Oral appliance therapy can greatly reduce sleep apnea severity for some people, and a subset may have near-complete resolution on testing. Many patients still need ongoing, nightly use to maintain results, and follow-up sleep testing is important to confirm control. [1][3][4]
Will it stop snoring?
Often, yes—but snoring reduction doesn’t always mean sleep apnea is fully treated. Objective follow-up testing can confirm effectiveness.
Is an oral appliance safe if I have TMJ?
It may be possible for some patients, but TMJ symptoms and jaw function should be evaluated and monitored. [2]
How long does it take to work?
Some people notice changes quickly, but optimal results often take weeks as the device is gradually adjusted. [2]
What if I have severe sleep apnea and can’t tolerate CPAP?
An oral appliance may be an alternative for some patients, sometimes with additional strategies. Objective re-testing is especially important in severe cases. [1][3]
Do over-the-counter mouthguards work for sleep apnea?
They aren’t considered reliable treatment for diagnosed OSA. Custom, clinician-guided therapy is generally preferred for safety, comfort, and measurable results. [2][4]
Bottom line: When in doubt, test and verify—objective data guides confident treatment decisions.
When to See a Specialist (and Next Steps)
Signs you should get evaluated
- Witnessed apneas or gasping/choking at night
- Excessive daytime sleepiness
- High blood pressure plus snoring or suspected breathing pauses
What to bring to your appointment
- Prior sleep study results (if you have them)
- CPAP history (if you’ve tried it)
- Dental history and any TMJ or bite concerns
Next step
If you’re exploring whether an oral appliance for sleep apnea fits your needs, the next step is typically a sleep evaluation and a discussion of treatment options based on your sleep study results.
Sleep and Sinus Centers of Georgia can help you understand your results and determine whether oral appliance therapy is an appropriate path. To get started, book an appointment: https://www.sleepandsinuscenters.com/
Bottom line: A brief evaluation can clarify your options—and help you start the treatment you’ll actually use.
Medical disclaimer
This article is for educational purposes and is not medical advice. Diagnosis and treatment decisions should be made with a qualified healthcare professional, based on your symptoms and sleep testing.
Disclaimer: This article is for educational purposes only and is not medical advice. Please consult a qualified healthcare provider for diagnosis and treatment.
Sources
[1] SleepApnea.org – Oral Appliance for Sleep Apnea: https://www.sleepapnea.org/treatment/oral-appliance-for-sleep-apnea/
[2] Cleveland Clinic – Oral Appliance Therapy: https://my.clevelandclinic.org/health/treatments/21129-oral-appliance-therapy-for-sleep-apnea
[3] PubMed Central review – Oral appliances vs CPAP, adherence and outcomes: https://pmc.ncbi.nlm.nih.gov/articles/PMC6956298/
[4] Harvard Health – Dental appliances for sleep apnea: https://www.health.harvard.edu/blog/dental-appliances-for-sleep-apnea-do-they-work-2021042822476
Don’t let allergies slow you down. Schedule a comprehensive ENT and allergy evaluation at Sleep and Sinus Centers of Georgia. We’re here to find your triggers and guide you toward lasting relief.








