Medical vs Surgical Treatment for Complex Chronic Sinusitis: Which Is Best?
If you’ve been dealing with months of congestion, facial pressure, post-nasal drip, or a reduced sense of smell, it’s natural to wonder about the medical vs surgical treatment for chronic sinusitis—especially when symptoms keep coming back. The reality is that chronic sinusitis (also called chronic rhinosinusitis, or CRS) is often an inflammatory condition with multiple contributors, so the “best” plan depends on what type of CRS you have, how severe it is, and how you’ve responded to treatment so far.
A helpful way to think about CRS is as a “swelling and drainage” problem. When the lining of the nose and sinuses stays inflamed, the sinus openings can behave like a pinched straw—airflow is limited, mucus doesn’t clear well, and symptoms linger.
Below is a patient-friendly overview used in discussions at Sleep and Sinus Centers of Georgia, designed to help you understand the options and prepare for a shared decision-making conversation with your ENT.

Quick answer (and why it isn’t one-size-fits-all)
The practical takeaway
Most people start with medical therapy, and surgery is considered when symptoms persist despite appropriate treatment (often called medically refractory disease) or when CRS is severe/complicated.
In other words: you typically don’t “skip” medical care. Even if surgery becomes the right next step, a strong medical routine often remains part of long-term control.
What research suggests (with an important caveat)
In studies of refractory chronic rhinosinusitis (CRS), endoscopic sinus surgery (ESS) often shows greater improvement in patient-reported symptoms and quality of life compared with continuing medical therapy alone. However, a recurring theme in research reviews is that the overall certainty of comparative evidence is frequently low to very low, so decisions should be individualized. [1,2]
A practical translation of that research nuance, many people do very well with ESS when they’re the right candidate, but the best plan still depends on your CT/endoscopy findings, CRS subtype, and goals (smell, breathing, fewer flares, less oral steroid use).
Bottom line: start with sound medical care; consider surgery when symptoms persist and testing confirms treatable disease.
What “complex chronic sinusitis” usually means
Chronic rhinosinusitis (CRS) definition
CRS generally means symptoms lasting 12 weeks or longer plus objective evidence of sinus inflammation on nasal endoscopy and/or a CT scan. [3] Learn more about chronic sinusitis (CRS) and how it’s defined: https://sleepandsinuscenters.com/chronic-sinusitis
This “symptoms + objective findings” combination matters. It helps separate true sinus inflammation from look-alike conditions that can feel similar (like migraine or chronic rhinitis).
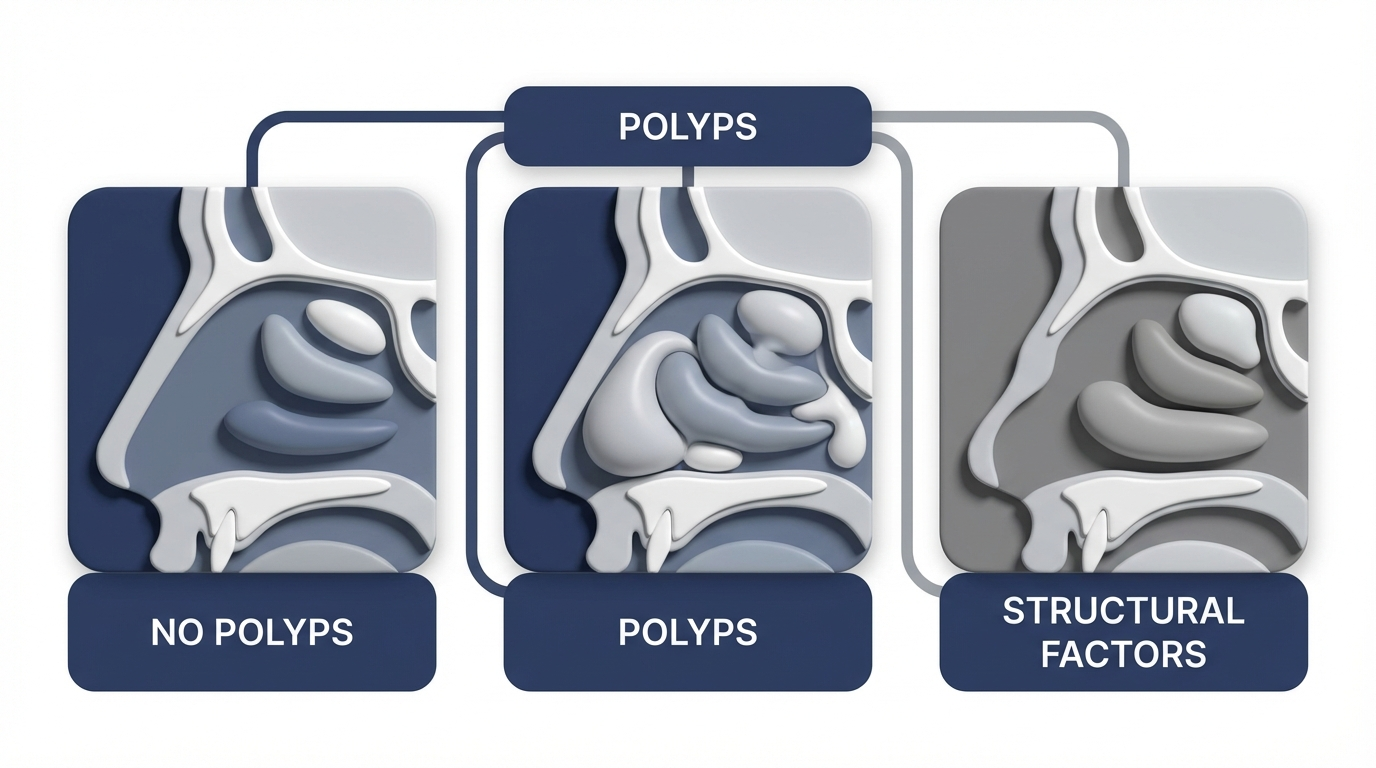
CRS types that affect treatment choices
“Complex” CRS isn’t one official diagnosis, but it often describes situations such as:
- CRS with nasal polyps (CRSwNP) vs. without nasal polyps (CRSsNP)
- Frequent flares or persistent symptoms despite treatment
- Prior sinus surgery with recurrent symptoms
- Significant anatomic blockage (narrow drainage pathways, septal deviation, turbinate enlargement)
- Coexisting asthma, aspirin-exacerbated respiratory disease (AERD), or other inflammatory conditions
- Less common drivers like immune deficiency or allergic fungal sinusitis (often needs specialist-level evaluation)
A clinician might call CRS “complex” when the pattern suggests it’s not just one simple issue to fix—more like overlapping layers (inflammation + anatomy + triggers).
Key idea: your CRS subtype and objective findings are what steer the best treatment plan.
Symptoms patients notice (and “red flags” that need prompt care)
Common CRS symptoms
People with CRS often report:
- Nasal congestion/obstruction
- Thick drainage or post-nasal drip
- Facial pressure/fullness
- Reduced smell and taste
- Cough, fatigue, and sleep disruption (often related to nasal blockage)
Many patients describe it as “always feeling like I’m getting over a cold,” even when they’re not acutely sick. Others notice the biggest impact at night—mouth breathing, dry throat, restless sleep, and waking up still congested.
Symptoms that should trigger urgent evaluation
Certain symptoms can suggest complications or a different diagnosis and typically warrant prompt medical evaluation, such as:
- Vision changes or severe swelling around the eye
- High fever, stiff neck
- Severe headache, confusion, or neurologic symptoms
If you ever feel like your symptoms are escalating quickly (especially around the eye), it’s appropriate to seek prompt evaluation rather than “waiting it out.” If symptoms worsen or do not improve as expected—even without these red-flag signs—schedule follow-up with your healthcare provider.
Don’t wait on rapidly worsening symptoms; even without red flags, persistent or worsening issues deserve timely evaluation.
Why chronic sinusitis happens (causes + risk factors)
Inflammation is often the main driver
CRS is frequently driven more by ongoing inflammation than by a persistent infection, which is why anti-inflammatory treatments play a central role. [3]
A common misconception is that CRS always equals “I need stronger antibiotics.” In reality, antibiotics can be helpful during specific bacterial flare-ups, but they’re not the foundation for long-term control in many CRS cases. [3]
Common contributors
CRS can be influenced by:
- Allergies / allergic rhinitis
- Viral colds triggering prolonged inflammation
- Asthma/AERD and nasal polyps
- Environmental irritants (smoke, pollution) and workplace exposures
As one clinician might put it: “For many people, we’re treating the inflammation that follows triggers—not just the triggers themselves.”
Anatomy and airflow/drainage problems
Physical factors can worsen symptoms or prevent sinuses from draining well, such as:
- Deviated septum
- Narrow sinus drainage pathways
- Turbinate enlargement
Think of the sinuses like rooms connected by small hallways. If the hallways are narrowed (by swelling, anatomy, or both), ventilation and drainage become harder—so symptoms build up more easily.
Less common but important
In some cases, CRS relates to:
- Immune deficiencies
- Certain autoimmune/vasculitic disorders
- Allergic fungal sinusitis
These scenarios are less common, but they can change the workup and long-term strategy—one reason persistent cases benefit from ENT-level evaluation.
Most CRS is inflammation-first; understanding your triggers and anatomy helps target the right treatment.
How ENTs diagnose “refractory” CRS before recommending surgery
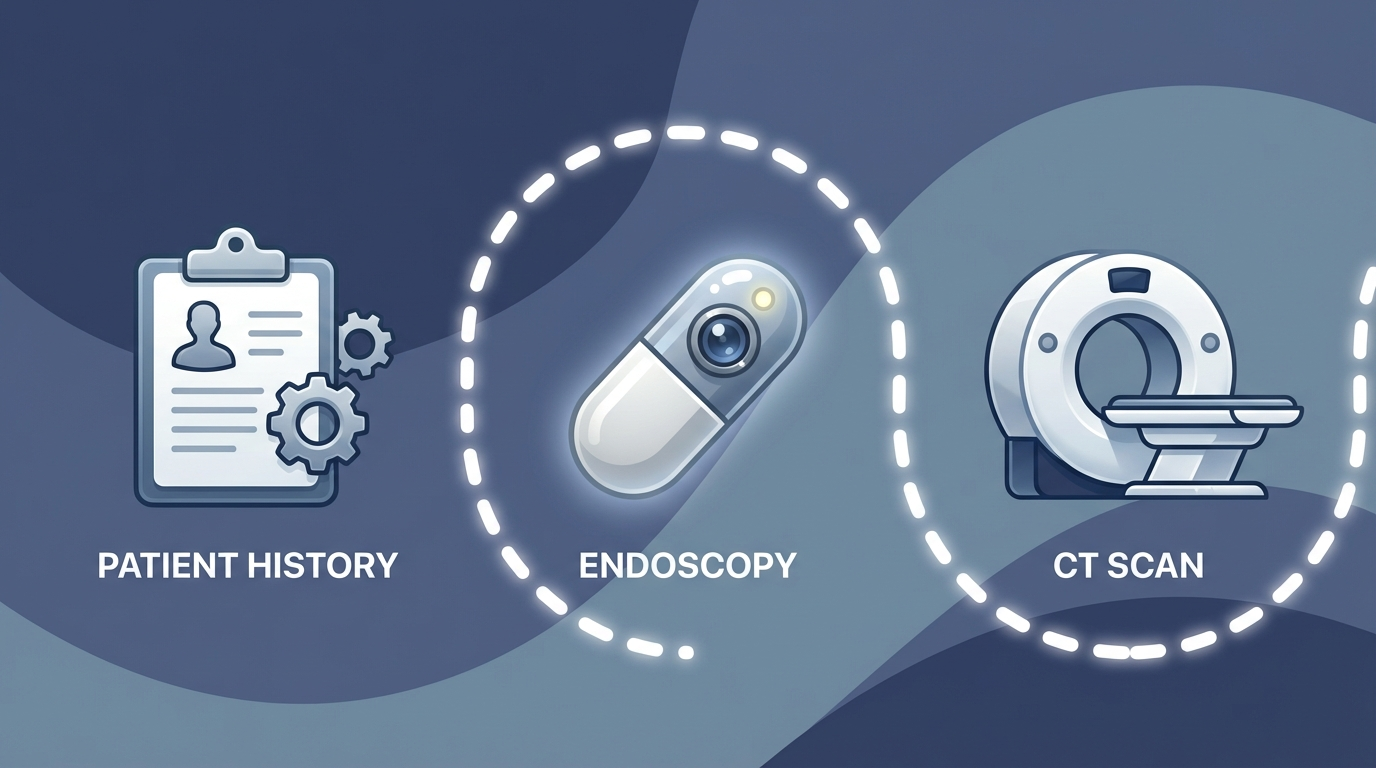
History + symptom scoring
Your clinician will usually review symptom duration, flare patterns, triggers, past antibiotics or steroid use, and impact on sleep and daily function.
Many practices also use standardized symptom questionnaires over time. The goal is simple: measure where you started, what you’ve tried, and whether you’re truly improving.
Nasal endoscopy
Endoscopy can help identify swelling, polyps, drainage, scarring, or structural blockage.
Patients often appreciate that endoscopy makes the discussion more concrete—moving from “how it feels” to “here’s what we can actually see.”
CT scan of the sinuses
A CT scan helps define the location and extent of disease and can clarify whether a surgical approach is likely to help. [3]
CT findings also help set expectations. For example, if CT shows multi-sinus inflammation plus blockage, opening the pathways may be more likely to help than if CT looks fairly clear.
Rule-outs that mimic sinusitis
Not every face-pressure or congestion problem is CRS. ENTs also consider common “look-alikes” such as migraine, TMJ disorders, dental sources, or chronic rhinitis without true sinus involvement.
This step can be a relief for patients: if it’s not CRS, you can stop chasing sinus treatments and focus on the real driver.
Clear symptoms plus clear endoscopy/CT evidence guide whether surgery makes sense.

Medical treatment options (first-line for most people)
Goal: reduce inflammation, improve drainage, and prevent flares—often using a combination approach. [3] For a broader overview, see our hub on chronic sinusitis treatments: https://sleepandsinuscenters.com/chronic-sinusitis-treatment
Saline irrigation (rinses)
Saline rinses can help clear mucus, allergens, and irritants, and they’re commonly used alongside nasal sprays. [3]
A useful analogy: rinses are like “washing the sidewalk” before you apply treatment. Clearing the surface can make it easier for topical medications to reach inflamed tissue consistently.
Intranasal corticosteroid sprays
These are a cornerstone of long-term CRS care to reduce swelling and inflammation. [3]
Technique matters. Many patients do better once they learn how to angle the spray to reduce drip-down-the-throat and improve delivery where inflammation is highest.
Short courses of oral steroids (selected patients)
Oral steroids may reduce inflammation quickly—especially in people with significant swelling or polyps—but they’re not a long-term maintenance strategy due to potential side effects. [3]
A common real-world use is “resetting” a major flare so that topical routines can work better afterward—while still minimizing repeated courses when possible.
Antibiotics (only when appropriate)
Antibiotics tend to be most useful for suspected bacterial exacerbations, rather than for baseline inflammatory CRS, and should be used only under healthcare provider guidance to avoid unnecessary use and resistance. [3]
If your symptoms briefly improve on antibiotics and then return, that can be a clue that inflammation and obstruction—rather than infection alone—are playing a bigger role.
Allergy-focused medications
When allergies contribute, options may include antihistamines, leukotriene modifiers, and targeted allergy management. [3]
This is especially important when congestion is seasonal, exposure-related, or paired with itchy/watery eyes and frequent sneezing.
Biologics for nasal polyps (for selected CRSwNP patients)
For some people with severe or recurrent polyps—especially those trying to reduce repeated oral steroid use—biologics for nasal polyps can be considered as part of a long-term strategy. [4]
For the right patient, the decision is often framed as a long-term control plan: symptom burden, polyp recurrence, asthma/AERD overlap, and how often oral steroids are needed.
What “maximal medical therapy” often means in real life
When ENTs say “maximal medical therapy,” they often mean consistent daily use of foundational treatments (commonly rinses plus topical steroids), addressing allergy triggers when relevant, and then reassessing symptoms with endoscopy/CT if problems persist.
A practical benchmark many patients relate to is consistency: not just “I tried it,” but “I used it correctly and regularly long enough to judge whether it truly helped.”
Consistency with rinses and topical steroids is the foundation of long-term CRS control.

Surgical treatment options (when medical therapy isn’t enough)
Endoscopic Sinus Surgery (ESS)
Endoscopic sinus surgery (ESS) uses small cameras and instruments to open blocked sinus pathways, remove diseased tissue or polyps when present, and improve sinus ventilation and drainage. A major goal is also to improve access for ongoing topical medications after surgery. If you want a step-by-step overview, see endoscopic sinus surgery (ESS): what patients should know: https://sleepandsinuscenters.com/blog/endoscopic-sinus-surgery-what-patients-should-know
In medically refractory CRS populations, studies often show greater improvement in quality of life and symptom scores after ESS compared with continued medical management alone. [1,2]
A patient-friendly way to summarize ESS is: it aims to make the sinus “pathways” more open so inflammation treatments can get where they need to go.
Balloon sinuplasty (selected anatomy/disease patterns)
Balloon sinuplasty uses a small balloon to dilate certain narrowed sinus openings. It may be an option for specific patterns of blockage, but it isn’t a fit for every case of complex chronic sinusitis—especially when there are extensive polyps, widespread inflammation, or multi-sinus disease. Learn more about balloon sinuplasty: https://sleepandsinuscenters.com/balloon-sinuplasty
Septoplasty and turbinate reduction (when obstruction is a big driver)
When nasal airflow limitation is a major contributor, septoplasty and/or turbinate reduction may be performed alone or combined with sinus procedures.
This comes up often when the main complaint is “I can’t breathe through my nose,” and the exam shows structural blockage in addition to (or instead of) sinus inflammation.
Surgery widens key pathways so medicines can work better; it complements, not replaces, good medical care.
Medical vs surgical—head-to-head comparison patients care about
Symptom relief & quality of life
Evidence in refractory patients suggests ESS can provide larger improvements in symptom and quality-of-life measures, but overall certainty across studies is often low/very low, so results vary by person. [1,2]
If your symptoms are severe, persistent, and clearly match CT/endoscopy disease, ESS is more likely to be part of a meaningful improvement story.
Medication use after treatment
Some studies report reduced need for oral antibiotics and oral steroids after ESS compared with continued medical management in refractory CRS groups. [1,2]
Importantly, this doesn’t mean “no medications.” Many patients still use rinses and topical steroids—just with fewer systemic “rescue” medications.
Work/school and daily functioning
Some evidence suggests fewer missed days after ESS in medically refractory populations. [2]
For many patients, that’s the deciding factor: fewer days knocked out by pressure, fatigue, and congestion is a quality-of-life win.
Costs and time
- Medical therapy: ongoing time, cost, and adherence demands
- Surgery: an upfront procedure and recovery period, plus continued long-term maintenance care
A helpful mindset is to compare ongoing burden (daily symptoms + repeated flare treatment) versus upfront investment (procedure + recovery) when surgery is appropriate.
Safety and risks
- Medical risks: side effects from steroids (especially oral forms), antibiotic side effects, antibiotic resistance concerns
- Surgical risks: bleeding, infection, scarring, anesthesia risks; rare but serious complications should be reviewed in detail with the surgeon
Your ENT should walk you through how your individual anatomy and health history influence risk, and what steps are taken to minimize it.
Match treatment to your goals, disease pattern, and tolerance for ongoing burden versus an upfront procedure.
Who should consider surgery for complex CRS?
Common signs you may be a surgical candidate
Surgery is often discussed when:
- Symptoms persist despite appropriate and consistent therapy (i.e., refractory chronic rhinosinusitis). [1,2,3]
- Endoscopy and CT show ongoing inflammation/blockage that matches the symptom pattern. [3]
- Exacerbations lead to repeated oral steroid/antibiotic courses. [1,2]
- Significant polyps affect breathing or smell (sometimes prompting a combined discussion of surgery and biologics). [4]
A practical “candidate” example: someone who’s diligent with rinses and topical steroids, still can’t breathe well, still can’t smell, and has CT evidence of blockage that aligns with symptoms.
Who may do well with continued medical therapy
Continued medical care may be a better fit when CT/endoscopy findings are mild, symptoms are dominated by allergies/rhinitis, foundational therapies haven’t been used consistently, or someone strongly prefers to avoid procedures.
In these situations, tightening the medical plan (and technique) can sometimes produce the improvement that felt out of reach before.
If you’re consistent with care yet still stuck—and imaging matches symptoms—surgery becomes a reasonable next step.
What to expect if you choose ESS (patient-friendly timeline)
Before surgery
Pre-op planning typically includes reviewing endoscopy/CT findings and clarifying realistic goals. Many patients are surprised to learn that ESS is often intended to make ongoing topical therapy work better, not replace it entirely.
You may also discuss whether septoplasty/turbinate reduction is needed at the same time if nasal airflow limitation is a major driver.
Recovery basics
Early congestion and crusting can be expected. Follow-up visits and a rinse routine are commonly part of post-op care.
A simple expectation-setting line many patients appreciate: “You may feel stuffy at first—even though we opened things up—because tissue needs time to calm down.”
Long-term maintenance
Even after ESS, many patients continue topical therapies to keep inflammation controlled—especially those with an inflammatory CRS subtype. [3]
Long-term success often looks like fewer flares, easier breathing, and better medication delivery—rather than “never having sinus symptoms again.”
Plan for short-term stuffiness, close follow-up, and long-term topical care to maintain results.
Lifestyle tips that help either path (medical or surgical)
Daily habits that reduce flares
- A consistent saline rinse routine
- Correct nasal spray technique
- Hydration and sleep support habits
These sound simple, but consistency is often the difference between “I tried everything” and “I finally found what works.”
Allergen/irritant control
- Avoid smoke exposure
- Improve indoor air quality when possible
- Manage known allergic triggers
If you’re frequently exposed to irritants, even excellent medical therapy can feel like it’s always playing catch-up.
When to seek re-evaluation
A reassessment is often helpful when symptoms worsen after initial improvement, flares become frequent, or any red-flag symptoms appear.
Small daily changes compound into fewer flares and better long-term control.
FAQs (SEO-friendly)
Is chronic sinusitis usually an infection?
Not usually. CRS is often primarily inflammation, while infections are more likely during flare-ups. [3]
If I get ESS, will I be “cured”?
ESS can significantly improve symptoms and quality of life in appropriate refractory cases, but many patients still benefit from ongoing topical therapy afterward. [1,3]
When is surgery “the best solution”?
Often when symptoms persist despite appropriate medical therapy and objective testing confirms treatable sinus disease. [1,2,3]
What if I have nasal polyps—do I need biologics or surgery?
It depends on severity, recurrence, coexisting asthma/AERD, oral-steroid burden, and personal preferences. Biologics for nasal polyps are an option for selected patients with CRSwNP. [4]
Does surgery reduce antibiotic and steroid use?
Some studies in refractory CRS populations report reduced oral antibiotic and steroid use after ESS compared with continued medical management. [1,2]
Balloon sinuplasty vs ESS—what’s the difference?
- Balloon dilation targets specific narrowed openings
- ESS is typically broader and may be used for more complex or extensive disease patterns
Shared decision-making checklist (help patients choose)
Questions to ask your ENT
- What CRS subtype do I have (with or without polyps)?
- What did my CT/endoscopy show, and does it match my symptoms?
- Looking back, what therapies have I used consistently, and for how long?
- What outcomes are realistic for me (breathing, smell, flare frequency, medication use)?
- What risks matter most given my anatomy and health history?
Goals-based decision
A practical way to approach the medical vs surgical treatment for chronic sinusitis is to prioritize your goals—such as faster symptom relief, fewer flare-ups, reducing oral steroid dependence, or minimizing missed work—then match those goals to the options supported by your CT/endoscopy findings and medical history.
Next step: If you’re dealing with persistent symptoms and want a clear plan based on endoscopy/CT findings, you can book an appointment with an ENT at Sleep and Sinus Centers of Georgia here: https://www.sleepandsinuscenters.com/
Bring your goals and questions—shared decision-making with your ENT leads to the most personalized plan.
References
1. Systematic review/meta-analysis: Surgery vs continued medical therapy for refractory CRS. https://pmc.ncbi.nlm.nih.gov/articles/PMC11193160/
2. Prospective comparative outcomes: ESS vs continued medical management. https://pubmed.ncbi.nlm.nih.gov/22736422/ and https://experts.arizona.edu/en/publications/medical-therapy-vs-surgery-for-chronic-rhinosinusitis-a-prospecti/
3. Mayo Clinic: Chronic sinusitis diagnosis & treatment overview. https://www.mayoclinic.org/diseases-conditions/chronic-sinusitis/diagnosis-treatment/drc-20351667
4. JACI: Biologics and CRSwNP context. https://www.jacionline.org/article/S0091-6749(16)31791-2/pdf
Medical disclaimer
This article is for general educational purposes only and is not a substitute for medical advice, diagnosis, or treatment. If you have urgent symptoms (such as vision changes, severe swelling around the eye, high fever, stiff neck, severe headache, confusion, or neurologic symptoms), seek prompt medical care.
This article is for educational purposes only and is not medical advice. Please consult a qualified healthcare provider for diagnosis and treatment.
Don’t let allergies slow you down. Schedule a comprehensive ENT and allergy evaluation at Sleep and Sinus Centers of Georgia. We’re here to find your triggers and guide you toward lasting relief.







