Inspire vs CPAP for Sleep Apnea: Which Treatment Is Better?
If you’ve been diagnosed with obstructive sleep apnea (OSA), it’s normal to wonder which treatment is “best”—especially when you hear about newer, mask-free options. The truth is that “better” depends less on the device and more on you: your sleep study results, your anatomy, your comfort with different therapies, and what you can realistically use night after night. Sleep specialists consistently emphasize that treatment selection is individualized and based on severity, tolerance, and preferences.
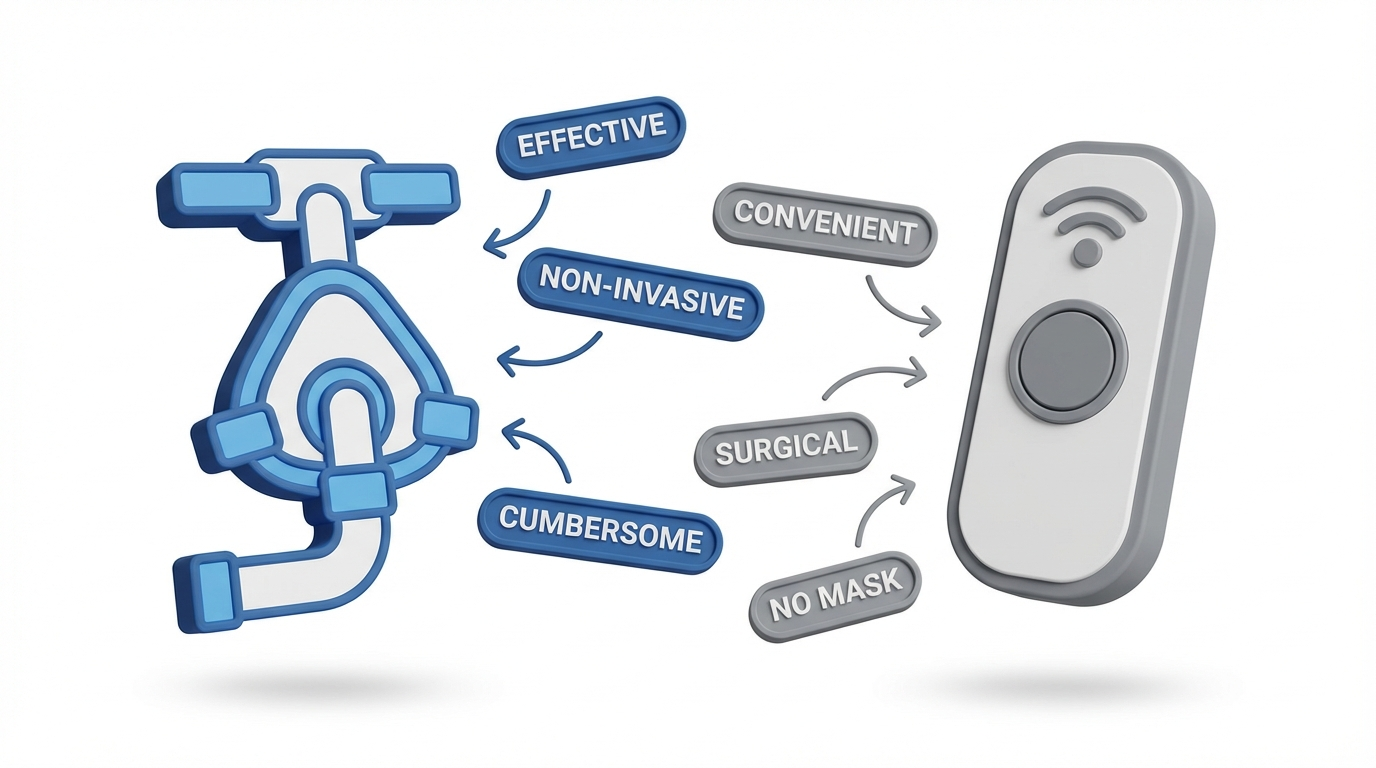
CPAP is a widely used first-line therapy for many people with OSA because it’s non-surgical, adjustable, and highly effective when used consistently. Inspire therapy (a sleep apnea implant that uses hypoglossal nerve stimulation) is typically considered after a documented, optimized CPAP trial shows intolerance or inability to use CPAP consistently enough to benefit.
A quick snapshot: CPAP is mask-based—it gently “splints” the airway open with air pressure. Inspire is mask-free—it helps keep the airway open by stimulating the nerve that controls tongue movement during sleep.
One way clinicians often frame it is simple: the right therapy is the one that reliably treats your breathing and fits into real life. If a treatment works perfectly “in theory,” but you can’t comfortably use it, you may not get the results you’re hoping for.
Bottom line: the “best” treatment is the one you can use safely, comfortably, and consistently.

Understanding Obstructive Sleep Apnea (OSA)
Obstructive sleep apnea happens when the upper airway repeatedly narrows or collapses during sleep, reducing airflow and disrupting normal sleep. Even if you don’t fully wake up, these interruptions can fragment sleep and contribute to daytime symptoms and long-term health risks.
Many patients are surprised to learn that OSA isn’t just about snoring. Snoring can be a clue, but the bigger issue is what’s happening behind the noise: repeated obstruction, oxygen dips, and frequent micro-arousals that keep sleep from being truly restorative.
Common Symptoms of Sleep Apnea
• Loud snoring
• Pauses in breathing, gasping, or choking during sleep
• Excessive daytime sleepiness, low energy, morning headaches, or brain fog
• Mood changes, irritability, or trouble concentrating
• High blood pressure or increased cardiovascular risk, which are associated with untreated OSA
A concrete example: someone may “sleep” eight hours but still wake up feeling unrefreshed, rely on caffeine to get through the day, or struggle with afternoon drowsiness—because their sleep quality is disrupted over and over.
What Causes OSA?
• Airway collapse during sleep as soft tissues relax
• Anatomy factors (jaw size/position, tongue position, enlarged tissues)
• Weight and neck circumference as risk factors (not a personal failing)
• Alcohol/sedatives and sleep position (especially back sleeping) which can worsen airway collapse
Think of the upper airway like a soft, flexible “tube.” When you’re awake, muscle tone helps keep it open. During sleep, those muscles relax, and in some people the airway becomes more likely to narrow—especially in certain positions or with certain anatomical factors.
If you want to better understand how severity is measured, see our guide on your AHI score and sleep apnea severity: https://sleepandsinuscenters.com/blog/ahi-score-explained-understanding-your-sleep-apnea-severity
Key takeaway: OSA is about repeated airway blockage and fragmented sleep—not just snoring.

CPAP Explained (Continuous Positive Airway Pressure)
A CPAP machine has been used for decades and remains a widely used first-line obstructive sleep apnea treatment.
How CPAP Works
CPAP delivers a steady flow of air through a mask to help keep the airway open during sleep. Because it directly prevents airway collapse, CPAP is often considered the “gold standard” when used consistently.
An easy analogy: CPAP works like a gentle air “brace” for the airway. It doesn’t force you to breathe—it simply keeps the passageway from pinching closed, so breathing can stay smooth and uninterrupted.
Who CPAP Is Best For
• Mild, moderate, or severe OSA
• People who prefer non-surgical, adjustable options
• Those able to commit to nightly use (and troubleshoot comfort issues as needed)
In real life, a lot of successful CPAP users don’t start out loving it. They get there by dialing in the mask, heated humidification, and settings until it feels manageable—and then it becomes routine, like brushing your teeth before bed.
Benefits of CPAP
• Non-surgical and reversible (you can stop without a procedure)
• Highly effective when used consistently and correctly
• Widely available and typically covered by insurance (coverage varies by plan)
Another practical benefit: CPAP settings can often be adjusted over time. If your needs change (for example, nasal congestion, weight changes, or different sleep positioning), your sleep team can usually troubleshoot without needing a new procedure.
Common CPAP Challenges (and Why People Quit)
Even though CPAP works well “on paper,” real-world success can be limited by comfort and adherence issues. Common barriers include:
• Mask discomfort, pressure marks, leaks, or claustrophobia
• Nasal congestion, dryness, or mouth dryness
• Noise, cleaning tasks, and travel hassles
• Inconsistent use (which can reduce overall benefit)
A common scenario: a patient uses CPAP for the first few hours of the night, then removes it half-asleep because the mask shifts or the mouth feels dry. The machine may be effective during use, but inconsistent wear time can limit overall improvement.
Lifestyle Tips to Improve CPAP Comfort & Success
Many CPAP problems are fixable with the right support and small adjustments. Addressing comfort and adherence barriers can make CPAP much more successful. Options to discuss with your care team include:
• Re-fitting the mask or trying a different mask style
• Using heated humidification and practicing nasal care routines
• “Desensitization” practice (wearing the mask briefly while awake)
• Pressure adjustments or comfort settings changes under supervision
For more ideas, see our guide on CPAP side effects and comfort tips: https://sleepandsinuscenters.com/blog/ent-care-for-people-who-use-cpap-machines
A simple rule: if CPAP is comfortable enough to use nightly, it’s hard to beat for effectiveness.

Inspire Therapy Explained (Hypoglossal Nerve Stimulation)
For some people—especially those who struggle with CPAP intolerance even after troubleshooting—Inspire therapy can be an alternative OSA treatment option.
What Inspire Is and How It Works
Inspire therapy is an implantable system designed to treat OSA by stimulating the hypoglossal nerve, which helps control tongue movement. During sleep, this stimulation can help keep the tongue from collapsing backward and blocking the airway. It’s used at night and typically turned on and off with a small remote. Inspire is commonly described as a mask-free alternative for people with moderate to severe OSA who cannot tolerate CPAP after a documented, optimized trial.
In practical terms, many patients like the simplicity: no mask to fit, no hose to manage, and no nightly cleaning routine for equipment. That convenience can make it easier to stick with treatment—especially for those who have tried CPAP and simply couldn’t make it work. Patient response varies, so individualized evaluation is important.
If you’d like a deeper overview, read our detailed post on Inspire therapy and hypoglossal nerve stimulation: https://sleepandsinuscenters.com/blog/inspire-hypoglossal-nerve-stimulation-a-101-guide-to-sleep-apnea-treatment
Who Inspire Is Best For (General Candidacy Guidelines)
• Moderate to severe OSA
• Documented CPAP intolerance or inability to use CPAP consistently after troubleshooting
• A thorough evaluation by a sleep specialist and ENT team to confirm candidacy, including sleep testing review and airway assessment
(Exact criteria vary, and candidacy is determined after appropriate testing and exam. A CPAP trial and optimization typically come first.)
Benefits of Inspire
• No mask or hose
• A simpler bedtime routine and easier travel logistics
• High patient satisfaction reported across many clinical settings, with the understanding that individual results vary
For people who travel frequently or share a bed with a partner who dislikes mask noise or airflow, the “no equipment on the nightstand” aspect can be a meaningful quality-of-life upgrade.
Downsides/Risks of Inspire to Consider
It’s also important to understand the tradeoffs. Many resources highlight the balance of mask-free convenience versus surgery and cost. Considerations include:
• Surgery is required, plus recovery time
• The battery will eventually require replacement (about 10–11 years on average, depending on model and usage), which involves a procedure
• Higher upfront costs; insurance coverage varies and often requires preauthorization, and some plans may deny coverage
• Not every airway anatomy or obstruction pattern is a good match for this sleep apnea implant
It can help to think of Inspire as a long-term, implanted tool that still needs periodic follow-up—more like a “device relationship” than a one-and-done fix.
In short: Inspire is a strong option for the right candidate who can’t use CPAP reliably, but it does involve surgery, cost, and ongoing follow-up.
Inspire vs CPAP: Side-by-Side Comparison (Patient-Friendly)
Below is a simplified comparison to help frame a conversation with your sleep specialist. This is educational—individual recommendations depend on your evaluation.
How it works:
• CPAP: Air pressure via mask keeps the airway open.
• Inspire: An implant stimulates the hypoglossal nerve to help keep the airway open.
Effectiveness:
• CPAP: Very effective when used correctly and consistently.
• Inspire: Effective in appropriately selected patients, especially with documented CPAP intolerance.
Daily comfort:
• CPAP: Mask fit, dryness, and leaks can affect adherence; heated humidification and mask changes often help.
• Inspire: No mask, but requires nightly device use, programming/titration visits, and comfort fine-tuning.
Lifestyle fit:
• CPAP: Requires cleaning, packing, and power access for travel.
• Inspire: Implanted, so travel is typically simpler (no equipment to pack).
Invasiveness:
• CPAP: Non-surgical and reversible.
• Inspire: Surgical implant; removable but involves procedures.
Cost and insurance:
• CPAP: Lower upfront costs with ongoing supply expenses.
• Inspire: Higher upfront costs; coverage criteria vary, preauthorization is common, and denials can occur.
Effectiveness (Real-World vs “On Paper”)
When people use CPAP nightly and it’s properly adjusted, it can be extremely effective. However, discomfort or inconsistent use can reduce real-world results. Inspire can be effective for appropriately selected patients—particularly those who can’t use CPAP consistently.
A useful way to compare: CPAP effectiveness is often limited by “Can I wear it?” while Inspire effectiveness is often limited by “Am I a good candidate?” Both questions are solvable, but they require different next steps.
Comfort and Daily Use
CPAP comfort often hinges on the right mask, humidification, and pressure settings. Inspire removes the mask from the equation, but it still requires follow-ups for optimization and routine use every night.
For example, someone with frequent nasal dryness may do much better on CPAP after adding heated humidification and changing mask style, while someone with persistent claustrophobia may still struggle even after multiple trials—making a mask-free option feel more realistic.
Convenience & Lifestyle Fit
If you travel frequently, share a bed, or dislike the routine of cleaning and packing equipment, lifestyle fit becomes a big part of the decision. This is one reason people compare Inspire vs CPAP so often: both can work, but they integrate into daily life differently.
Safety & Reversibility
CPAP is non-invasive and reversible. Inspire involves surgery and implanted hardware; while it can be removed, that still means additional procedures.
Cost & Insurance Considerations
CPAP usually has a lower upfront cost but includes ongoing expenses (masks, filters, tubing). Inspire is often higher upfront and may require insurance preauthorization and meeting specific criteria; coverage and out-of-pocket costs vary.
Practical takeaway: compare not just “which works,” but “which will I realistically use every night given my evaluation and lifestyle.”

How a Sleep Specialist Helps You Choose the Right Option
Choosing between Inspire and CPAP shouldn’t be a solo decision. Multiple clinical resources emphasize working with a specialist rather than self-selecting a treatment.
Many patients come in feeling like they must “pick one.” In reality, the process often looks more like stepwise problem-solving: confirm severity, try CPAP with real troubleshooting support (when appropriate), and then consider alternatives if CPAP can’t be used consistently enough to help.
Key Factors Your Provider Will Consider
• OSA severity (e.g., measured by AHI), oxygen saturation levels, and symptom burden
• Your CPAP trial history and what troubleshooting has already been attempted
• Airway anatomy and the pattern of collapse
• Health conditions and surgical risk
• Your preferences (mask-free vs non-surgical) and lifestyle needs
Bringing specifics helps. Instead of “CPAP didn’t work,” it’s useful to share details like: “I tried two masks, but I woke up with dry mouth every night,” or “I removed it unconsciously after an hour,” or “I travel weekly and struggled to keep up with cleaning.” Those details guide better solutions.
What the Evaluation Process Might Look Like
• Reviewing your sleep study (home or lab)
• A CPAP trial with troubleshooting support when appropriate
• If considering Inspire therapy: additional ENT evaluation and candidacy testing
Short version: let your sleep team match therapy to your sleep data, airway anatomy, and what you can stick with long term.
Other Treatment Options (If Neither Feels Right)
CPAP and Inspire aren’t the only OSA treatment options.
Oral Appliance Therapy
Oral appliances are often used for mild to moderate OSA, and sometimes for people who are CPAP-intolerant. Learn more about oral appliance therapy and oral appliance vs CPAP: https://sleepandsinuscenters.com/blog/oral-appliance-vs-cpap-which-is-right-for-you
Lifestyle & Behavioral Treatments
Depending on the situation, a care plan may also include:
• Weight management (if applicable) and regular exercise
• Sleep position strategies
• Avoiding alcohol close to bedtime
• Managing nasal obstruction or allergies
These aren’t “quick fixes,” but they can meaningfully support whichever primary therapy you use—especially when the goal is steady, long-term control of OSA.
Surgical Options Beyond Inspire
There are other ENT-directed procedures that may be considered in select cases. As with any obstructive sleep apnea treatment, the right approach depends on individualized evaluation.
Think of OSA care as a toolbox—most people do best with the single option they can use consistently, sometimes supported by lifestyle steps.
FAQs
Is Inspire better than CPAP?
“Better” depends on OSA severity, CPAP tolerance, airway anatomy, and personal priorities. For many people, CPAP remains the first option; Inspire may be a strong alternative when a documented, optimized CPAP trial shows true intolerance.
What if CPAP works—but I hate wearing the mask?
It may help to revisit mask type, fit, heated humidification, and comfort settings. Some people do much better after targeted troubleshooting and support.
Who qualifies for Inspire therapy?
In general, Inspire is considered for moderate to severe OSA with documented CPAP intolerance, plus specialist evaluation and candidacy testing.
Does Inspire cure sleep apnea?
Inspire therapy treats OSA by reducing airway obstruction during sleep. Ongoing follow-up and monitoring are still important, and outcomes vary by person.
How long does Inspire last?
Battery life varies by model and usage; many patients can expect around 10–11 years before replacement is needed, which involves a procedure.
Can I travel with CPAP or Inspire?
You can travel with either. CPAP requires packing equipment, planning for power, and cleaning; Inspire is implanted, so travel routines are often simpler.
Remember: responses to any therapy vary—work with your provider to set expectations and plan follow-up.
Conclusion: The Best Treatment Is the One You’ll Actually Use
In the conversation about Inspire vs CPAP, the most important point is consistency. CPAP is first-line for a reason: it’s non-surgical and highly effective when used regularly. Inspire therapy can be an excellent option for people with moderate to severe OSA who have true CPAP intolerance and meet candidacy criteria.
If you’re unsure which direction makes sense, the next step is a personalized review of your sleep study results and your day-to-day needs. That conversation can clarify whether you’re more likely to succeed with CPAP optimization, Inspire candidacy testing, or another approach.
Ready to talk through your options? Book an appointment with Sleep and Sinus Centers of Georgia: https://sleepandsinuscenters.com/appointments
If you’re not local, consult a qualified sleep specialist in your area to review your study and treatment options.
Consistency and a personalized plan are what turn “treatment” into better sleep and better days.
References
1: Sleepless in Arizona. “Inspire Implant vs CPAP for Treating Sleep Apnea.” https://sleeplessinarizona.com/inspire-implant-vs-cpap-for-treating-sleep-apnea/
2: Iowa City ASC. “CPAP vs Inspire Therapy (PDF).” https://iowacityasc.com/wp-content/uploads/2024/02/CPAP-vs-Inspire-Therapy.pdf
3: Sleep Better Columbus. “Exploring Sleep Solutions: Oral Appliances vs Inspire vs CPAP Machines.” https://sleepbettercolumbus.com/exploring-sleep-solutions-oral-appliances-vs-inspire-vs-cpap-machines/
4: Collin County ENT. “CPAP vs Inspire Implant: Which Is Right for You?” https://collincountyent.com/cpap-vs-inspire-implant-which-is-right-for-you/
5: Pulmonary & Sleep Health. “Inspire Therapy vs CPAP: Choosing the Right Sleep Apnea Solution for Your Lifestyle.” https://pulmonaryandsleephealth.com/inspire-therapy-vs-cpap-choosing-the-right-sleep-apnea-solution-for-your-lifestyle/
This article is for educational purposes only and is not medical advice. Please consult a qualified healthcare provider for diagnosis and treatment.
Don’t let allergies slow you down. Schedule a comprehensive ENT and allergy evaluation at Sleep and Sinus Centers of Georgia. We’re here to find your triggers and guide you toward lasting relief.








