Persistent Chronic Sinusitis Despite Medical Therapy: Next Treatment Options
If you’ve been doing the “standard” routine—saline rinses, nasal sprays, maybe a round (or several) of medications—and you still feel congested, pressured, or constantly drained, you’re not alone. Chronic rhinosinusitis (CRS), often called chronic sinusitis, is a long-lasting condition where symptoms persist because the underlying problem is frequently ongoing inflammation, not simply an infection that clears with antibiotics (AAFP). When you’re dealing with persistent symptoms despite medical therapy (sometimes called “failed chronic sinusitis medical management”), the next step is usually a more precise diagnosis—followed by targeted therapies, procedures, or (for some patients) surgery or advanced medications. For a refresher on CRS fundamentals, see our overview of chronic sinusitis.
CRS basics (and why it’s different from an acute sinus infection)
CRS is generally defined as sinus-related symptoms lasting 12 weeks or longer, along with objective evidence of inflammation (found on exam or imaging). Unlike an acute sinus infection that may clear after a short period, CRS is often driven by inflammatory pathways and ongoing triggers. That’s one reason repeated antibiotics often don’t solve the root problem (AAFP). A helpful way to think about it: an acute infection can be like a “small fire” that flares and goes out. CRS is more like a “smoldering” inflammatory process that keeps reactivating—sometimes with infections layered on top, but not always. For a plain-language review of symptoms, causes, and first-line care, visit chronic sinusitis.
– In short: CRS is usually an inflammatory problem first, not just a recurring infection.

What “optimal medical therapy” usually includes
- Nasal saline irrigation (often daily; sometimes twice daily)
- Intranasal corticosteroid sprays used consistently (and with correct technique)
- In selected cases, a short course of oral steroids, often when nasal polyps are present (provider-directed)
- Antibiotics only when bacterial infection is strongly suspected—not automatically for every CRS case (AAFP; Medscape)
One ENT perspective you may hear is: if medication can’t reach the inflamed tissue—or if inflammation is constantly re-triggered—then more of the same won’t change the outcome. That’s why how treatments are used (dose, delivery, technique, consistency) often matters as much as which treatment you’re using. For a side-by-side look at medical options and how they’re used, see chronic sinusitis treatment options.
– Bottom line: Getting the basics right (and delivered to the right place) is essential before moving on.
How common is non-response?
It’s not unusual for symptoms to persist even after a solid course of medical therapy. In research, a substantial portion of patients report inadequate relief with medication alone (PMC; SAGE). This doesn’t mean medications are ineffective; it reflects that CRS is complex and often requires stepwise care that may include procedures or surgery to improve medication delivery and long-term control.
– Key takeaway: If meds haven’t fully solved it, you’re not alone—and you still have options.
Symptoms that suggest you may need the next level of care
Classic CRS symptoms
- Nasal congestion or obstruction
- Thick mucus or post-nasal drip
- Facial pressure or pain
- Reduced smell (and sometimes taste) (AAFP)
Quality-of-life signs that matter clinically
CRS isn’t just “a stuffy nose.” It can affect daily functioning, especially when sleep and concentration are impacted. Signs that often prompt escalation include:
- Poor sleep, fatigue, or “brain fog”
- Frequent flare-ups
- Repeated need for oral steroids or antibiotics over time
A concrete example: if you can breathe “okay” some days but still wake up unrefreshed, lose your sense of smell for weeks at a time, or need multiple urgent-care visits in a year, that’s often a signal to move beyond routine management. You can read more about timing and decision points in when to see an ENT.
– In brief: If symptoms keep disrupting your life, it’s reasonable to move to specialty care.
Red flags—when to seek urgent care (not routine CRS)
- Vision changes
- Significant swelling around the eyes
- High fever
- Stiff neck, severe headache, confusion
– If any of these occur, seek urgent evaluation rather than routine follow-up.
Why treatment fails: common underlying causes (and what they mean)
Understanding why symptoms persist is key—because the best next step depends on the driver. Two people can share the same complaint (“I’m always congested”) but have very different underlying causes and therefore different best-fit treatments.
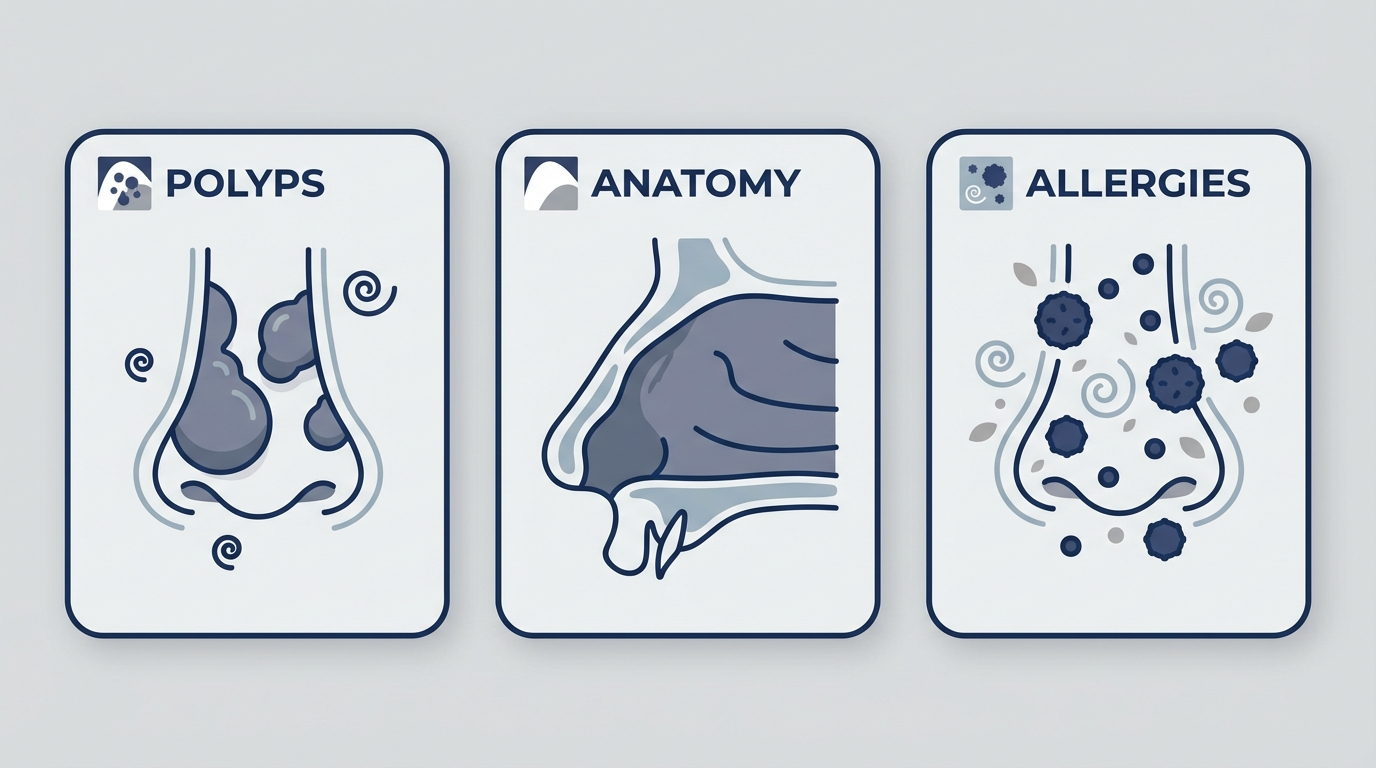
Nasal polyps and severe inflammation
Nasal polyps can physically block airflow and drainage, and they may also make it harder for topical medications to reach where they need to work (Medscape). Patients often describe this as, “It feels like my nose is permanently swollen shut,” or “Sprays don’t seem to go anywhere.” When polyps are present, the plan often shifts toward improving access and controlling inflammation more aggressively.
– In short: Polyps add both mechanical blockage and inflammation—often requiring a step-up in care.
Anatomical blockage (deviated septum, narrow drainage pathways)
Medication can reduce swelling, but it can’t always overcome structural narrowing or blockage. In these cases, procedures designed to improve sinus drainage may be considered. Think of it like trying to rinse a sink with a partially clogged drain: you can run water (medication), but if the passage is too narrow, the system still backs up. Endoscopy and imaging help clarify whether anatomy is a major limiting factor.
– Translation: If the “plumbing” is tight, improving the passage can make medicines work better.
Allergies and environmental triggers
Allergic inflammation can keep the nose and sinuses chronically reactive. That’s why evaluation sometimes includes identifying environmental triggers and considering allergy-directed strategies (AAFP).
– Takeaway: Calming allergy-driven inflammation can reduce CRS flare-ups.
Asthma/AERD and “united airway disease”
CRS—especially CRS with nasal polyps—commonly overlaps with asthma and related inflammatory conditions. These connections can influence which treatments are most effective long-term (PMC). In practice, this overlap can look like sinus symptoms flaring when asthma flares, or recurring polyp symptoms alongside wheezing. Coordinated management can matter.
– Bottom line: Treating the nose and lungs together often helps both.
Biofilms, chronic infection, or resistant organisms (selected cases)
Not every CRS case is infectious. But when infection is suspected in persistent or severe cases, clinicians may consider culture-directed therapy rather than repeated “guess-based” antibiotics (Medscape).
– Practical point: When infection is part of the picture, targeted treatment works better than repetition.
Next step after medical therapy falls short: See an ENT (otolaryngologist)
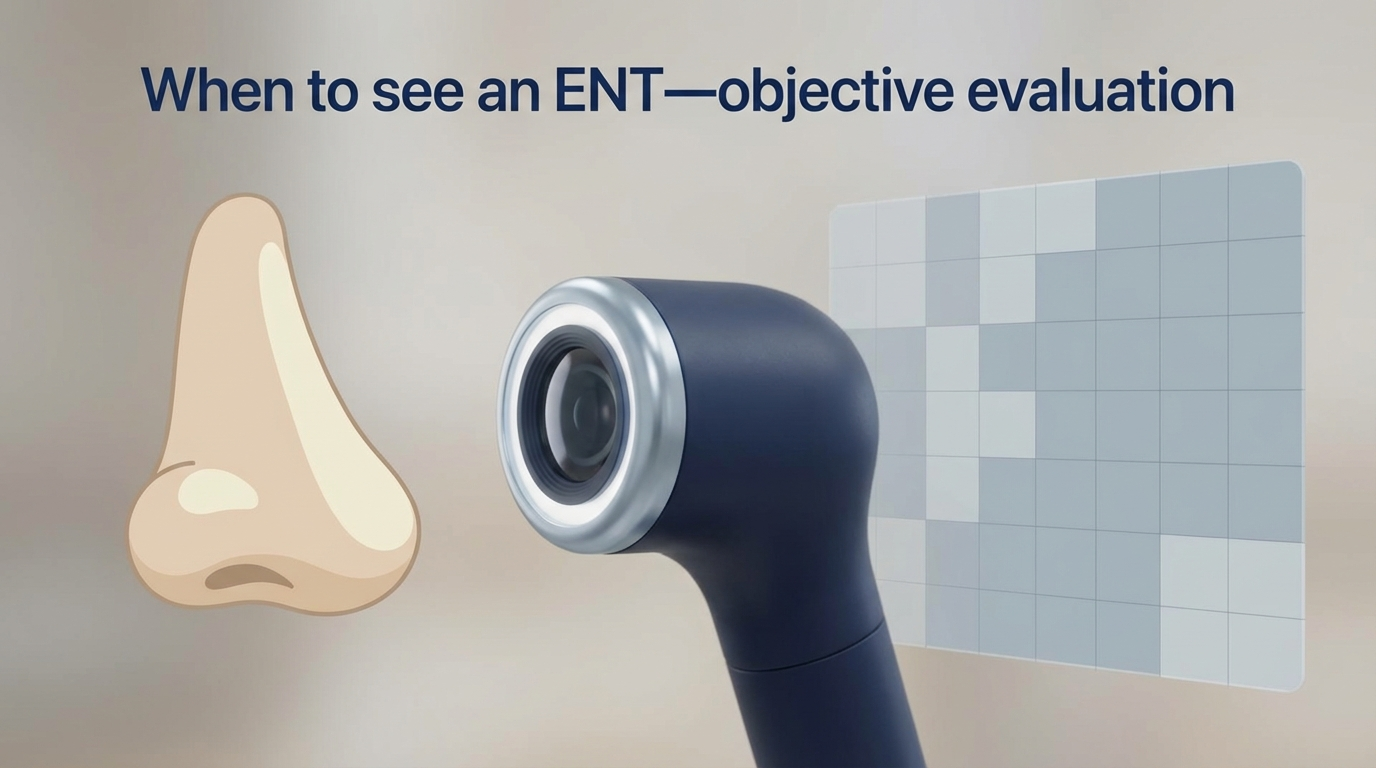
When persistent symptoms despite medical therapy become the pattern, an ENT evaluation can be a turning point—because it adds objective testing and more specialized options.
What the ENT evaluation typically includes
A typical visit may include:
- A detailed history (symptom timeline, flare patterns, medication trials, allergy/asthma history)
- Nasal endoscopy (an in-office exam using a small camera) to look for polyps, swelling, and drainage patterns (AAFP)
Many patients find it reassuring to finally “see what’s going on,” especially after months of symptoms that feel invisible from the outside. You can also learn more about timing in when to see an ENT.
– In short: Objective findings guide the right next step.
When imaging helps (sinus CT)
A sinus CT scan is commonly used to map anatomy and show the extent of sinus inflammation or blockage, especially when procedure or surgery is being considered (AAFP).
– Bottom line: CT helps tailor the plan to your unique anatomy and disease pattern.
Why referral matters
Persistent symptoms despite appropriate therapy are a common reason to escalate care, since next-step options (including procedures and surgery) depend heavily on endoscopy and CT findings (AAFP). For a deeper dive into care pathways, see chronic sinusitis treatment options.
– Key idea: The treatment that works best depends on what endoscopy and CT reveal.
Treatment options after medical therapy fails (patient-friendly guide)
Even when it feels like “I’ve tried everything,” clinicians often revisit the basics first—because technique and delivery matter. A small adjustment (for example, how you angle a spray or the volume used in irrigation) can make a meaningful difference for some patients.
Step-up medical options your clinician may consider
- Confirming correct spray technique and consistency
- Considering high-volume steroid irrigation in selected cases (provider-directed)
- Short courses of oral steroids, often for nasal polyps (provider-directed)
- Culture-directed antibiotics only for selected cases where bacterial infection is suspected (Medscape)
To explore these pathways in one place, visit chronic sinusitis treatment options.
– Takeaway: Fine-tuning meds and delivery can boost results before moving to procedures.
Minimally invasive procedures and surgery: what’s next and who benefits?
When persistent symptoms are linked to blockage, polyps, or anatomy that limits drainage and medication delivery, procedures may be discussed. The goals are to improve airflow/drainage and make ongoing topical therapy more effective.
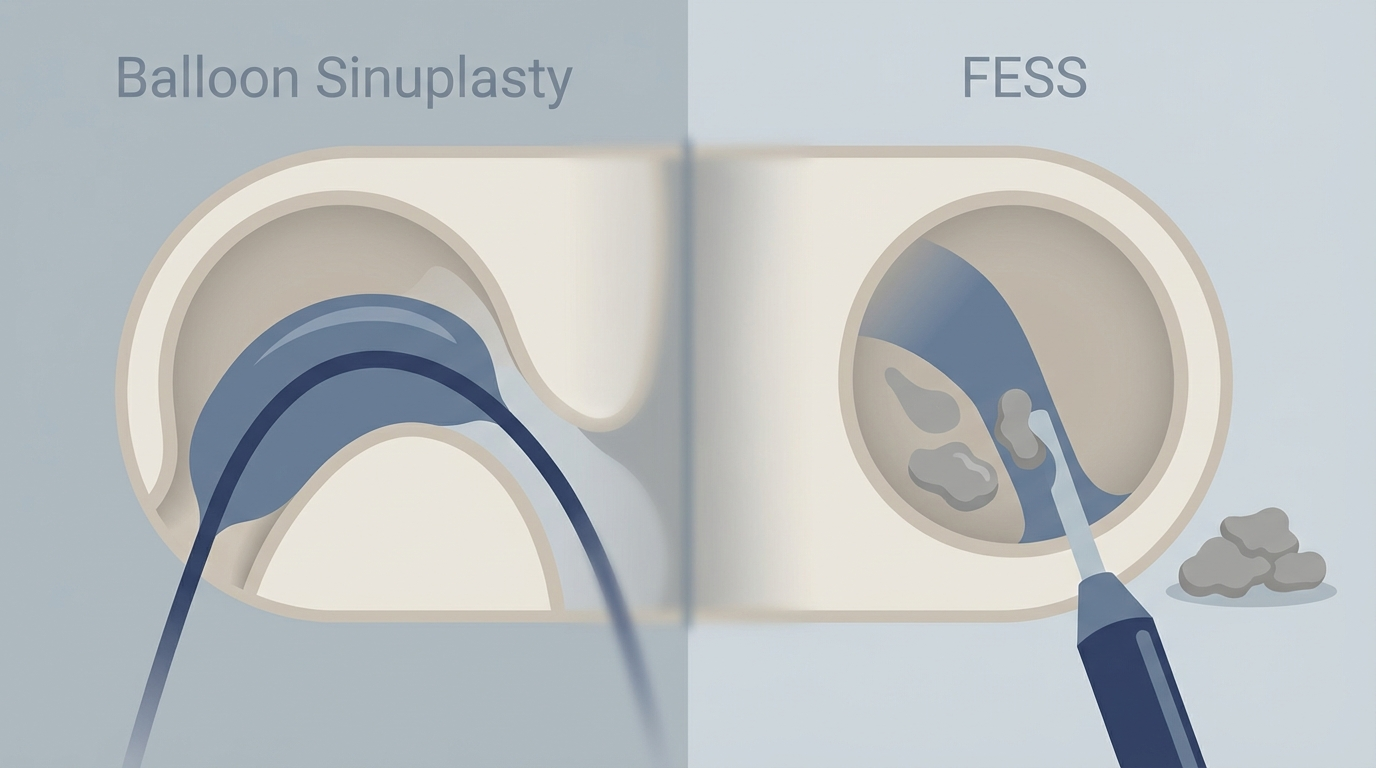
Balloon sinuplasty (less invasive option)
Balloon sinuplasty uses a small balloon to gently dilate certain sinus drainage pathways. It can be a fit for selected patients—often depending on which sinuses are involved and what the CT scan shows (Medscape). Learn more about balloon sinuplasty and who may be a candidate.
– In brief: Balloon dilation can open targeted pathways with minimal tissue removal.
Functional Endoscopic Sinus Surgery (FESS)
FESS is an endoscopic procedure that removes obstruction (such as inflamed tissue or polyps) and improves ventilation and drainage. It’s commonly considered after medical therapy doesn’t provide adequate relief—especially when endoscopy/CT shows more extensive disease (AAFP).
– Key point: FESS reshapes the “drainage system” so medicines can reach where they need to work.
What recovery and follow-up usually involve
Whether someone has a procedure or surgery, ongoing care often remains important. Follow-up may include saline rinses, topical medications, and in-office evaluations to support healing and long-term control. Because CRS is a chronic inflammatory condition, surgery is usually part of a management plan rather than a guaranteed permanent cure (Medscape).
– Bottom line: Surgery helps many people—but maintenance care remains essential.
Risks/benefits discussion (patient-centered)
Every intervention has potential benefits and risks. In CRS, decisions typically weigh:
- Symptom burden and quality-of-life impact
- CT/endoscopy findings
- CRS subtype (with or without polyps)
- Other conditions like asthma or aspirin sensitivity
Shared decision-making is key—especially when choosing between continued medical optimization, in-office procedures, or surgery.
– Takeaway: The best choice balances your goals, findings, and overall health picture.

Advanced therapy for severe CRS with nasal polyps: Biologics
What biologics are (simple explanation)
Biologics are prescription-only, injectable monoclonal antibody medications that target specific immune signals driving inflammation. They’re used in certain patients with chronic rhinosinusitis with nasal polyps (CRSwNP) and require specialist evaluation and monitoring.
– In short: Biologics selectively calm the immune pathways that drive polyp-prone inflammation.
Who may qualify
Biologics are typically considered for severe CRSwNP that persists despite standard therapies, and sometimes even after surgery—especially when asthma or aspirin-exacerbated respiratory disease (AERD) is also part of the picture (PMC).
– Key point: Biologics are reserved for tougher, polyp-heavy disease—often with asthma overlap.
Pros/cons patients should know
Potential benefits can include improved smell, reduced polyp size, and fewer flare-ups for some patients—but considerations include long-term planning, insurance coverage, injection schedules, and monitoring (PMC).
– Bottom line: Biologics can be transformative for some, but require a long-term plan.
Lifestyle tips and home care that still matter (even after escalation)
Even if you move beyond first-line therapy, daily habits still influence outcomes—especially because CRS management often depends on keeping baseline inflammation under control between flares.
Daily routines that improve outcomes
- Consistent saline irrigation (using safe water practices)
- Reducing exposure to irritants like smoke and strong fragrances
- Managing indoor air (balancing humidity; addressing dust or mold when relevant)
– Takeaway: Small daily steps add up—especially with a long-term condition like CRS.
Allergy control strategies if allergies are part of your CRS
Allergy testing and targeted treatment may be part of a comprehensive plan when allergies contribute to chronic inflammation (AAFP).
– In short: Treating allergies reduces the “fuel” for sinus inflammation.
Managing comorbid asthma
Because upper and lower airway inflammation often overlap, coordinating care can matter—especially for patients with asthma plus nasal polyps (PMC).
– Key idea: Better asthma control can support better sinus control, and vice versa.
FAQs
Why don’t antibiotics fix my chronic sinusitis?
Because CRS is often driven by inflammation more than infection. Antibiotics may help when a bacterial infection is present, but they aren’t a universal solution for chronic inflammation (AAFP).
When should I see an ENT for chronic sinusitis?
Persistent symptoms despite appropriate therapy, frequent flare-ups, significant smell loss, or suspected polyps are common reasons to consider evaluation (AAFP). Learn more in when to see an ENT.
Is balloon sinuplasty or FESS better?
It depends on anatomy, extent of disease, presence of polyps, and CT findings. Some patients are good candidates for balloon dilation, while others benefit more from FESS (Medscape). Explore options in chronic sinusitis treatment options.
Can CRS come back after surgery?
Symptoms can recur—especially in inflammatory CRS with polyps or allergy overlap—so ongoing topical therapy and follow-up are often part of long-term control (Medscape).
Are biologics a replacement for surgery?
Sometimes biologics are used after surgery, and sometimes they’re used when surgery isn’t preferred or feasible. The best fit depends on severity and CRS type (PMC).
– Bottom line: There isn’t a single “best” approach—your plan should be personalized.
Conclusion: You have more options than “just keep trying meds”
If you’re frustrated by persistent chronic sinusitis despite medical therapy, you’re not out of options—it usually means the next step is a clearer diagnosis and a more personalized plan. ENT evaluation (often including endoscopy and CT imaging) can help identify whether nasal polyps, anatomy, allergies, asthma overlap, or other factors are driving symptoms—and which combination of medical therapy, procedures, surgery, or biologics fits best. To explore next steps, learn more about chronic sinusitis and chronic sinusitis treatment options at Sleep and Sinus Centers of Georgia. Ready to get answers? You can book an appointment through https://www.sleepandsinuscenters.com/ to discuss your symptoms, prior treatments, and next-step options with a specialist.
– Final thought: The right diagnosis opens the door to the right treatment.
This article is for educational purposes only and is not medical advice. Please consult a qualified healthcare provider for diagnosis and treatment.
Don’t let allergies slow you down. Schedule a comprehensive ENT and allergy evaluation at Sleep and Sinus Centers of Georgia. We’re here to find your triggers and guide you toward lasting relief.








