Evidence-Based CPAP Alternatives That Actually Work for Sleep Apnea
CPAP is a highly effective treatment for obstructive sleep apnea (OSA)—but it’s not the only option. If you’ve tried CPAP and struggled with comfort, leaks, pressure, or just couldn’t sleep with it, there are evidence-based CPAP alternatives that can meaningfully reduce breathing disruptions and improve daytime symptoms. The key is matching the option to your sleep apnea pattern, anatomy, and severity—then confirming it’s actually working with follow-up data, not guesswork. Sources: Sleep Foundation (2025); SleepApnea.org (2025)
Quick Take—Yes, There Are Real CPAP Alternatives (But Not All Work the Same)
The goal of treatment: keep the airway open and protect oxygen levels
Most treatments aim to prevent the throat airway from narrowing or collapsing during sleep—so breathing stays steady and oxygen levels remain supported. A simple way to picture it: your airway can behave like a soft tube that’s more likely to kink when muscles relax at night. Treatment is about keeping that tube stable. Source: Sleep Foundation (2025)
Why “best alternative” depends on your sleep apnea type and severity
Obstructive sleep apnea (airway collapse) is most common, but central sleep apnea (brain signaling issue) and mixed sleep apnea can also occur. Because treatments work differently depending on the cause, clinical evaluation and appropriate testing matter before switching therapies. Source: Sleep Foundation (2025)
Conclusion: The right therapy is the one matched to your diagnosis—and proven by follow-up testing.
Sleep Apnea Symptoms You Shouldn’t Ignore
Nighttime symptoms
- Loud, persistent snoring
- Witnessed pauses in breathing
- Gasping or choking awakenings
- Frequent waking or restless sleep
Daytime symptoms
- Morning headaches
- Dry mouth on waking
- Brain fog or concentration issues
- Mood changes/irritability
- Excessive sleepiness
When symptoms are urgent
Severe daytime sleepiness (including drowsy driving risk) or suspected oxygen drops are important signals to seek prompt evaluation and testing. If you’re nodding off at stoplights, waking up gasping, or your bed partner notices repeated breathing pauses, don’t wait and see. Source: Sleep Foundation (2025)
Conclusion: If sleepiness or breathing pauses are significant, get evaluated promptly.
What Causes Obstructive Sleep Apnea (OSA)?
Anatomy and airway crowding
OSA often involves a combination of airway anatomy and sleep-related muscle relaxation. Contributors include the tongue/base of tongue, soft palate, tonsils/adenoids (when enlarged), and nasal obstruction that increases breathing resistance. This is why two people with the same AHI can feel very different—and why the right therapy often depends on where the airway is collapsing. Sources: Harvard Health (2020); SleepApnea.org (2025)
Risk factors that increase collapse
- Weight gain/obesity
- Alcohol or sedative use (especially near bedtime)
- Sleeping on the back
- Aging-related changes in muscle tone
Sources: Harvard Health (2020); Sleep Foundation (2025)
Why diagnosis matters before switching treatments
Choosing among alternatives to CPAP is much easier when you know your severity and pattern. Your AHI is a starting point. If you’re still in the diagnosis phase, consider whether you need a home sleep test or lab study. Sources: Harvard Health (2020); SleepApnea.org (2025)
Conclusion: Understanding your anatomy, severity, and sleep study details makes every treatment decision more accurate.
Why Some People Can’t Tolerate CPAP (and What to Try Before Quitting)
Common CPAP problems
- Pressure discomfort (especially when falling asleep)
- Mask leaks or skin irritation
- Claustrophobia or can’t relax feeling
- Dry mouth, nasal dryness, or congestion
CPAP optimization checklist
Before moving on, many people benefit from mask refitting, humidification changes, pressure setting review, and nasal care support. Sometimes the issue isn’t PAP therapy itself—it’s the setup. Source: Sleep Foundation (2025)
If you still can’t tolerate CPAP, these alternatives are evidence-based
If optimization still doesn’t work, the options below represent the most evidence-supported CPAP alternatives currently used for OSA. Sources: Sleep Foundation (2025); SleepApnea.org (2025)
Conclusion: Fix the easy CPAP issues first—then choose a proven alternative if comfort still blocks success.
Evidence-Based CPAP Alternatives (Ranked by How They Work)

1) Oral Appliances (Especially Mandibular Advancement Devices)
A mandibular advancement device is a custom oral appliance that gently moves the lower jaw forward during sleep to increase space behind the tongue and reduce airway collapse. Sources: Sleep Foundation (2025); SleepApnea.org (2025); PMC evidence reviews
Who they help most: mild to moderate OSA or people who cannot tolerate CPAP; popular with travelers or those wanting a quieter, simpler setup. Sources: SleepApnea.org (2025); PMC summaries
Expected results: many improve; roughly a subset may achieve near-complete resolution under proper use—results vary and require follow-up testing. Good real-world adherence due to portability. Sources: PMC10684110; PMC9584565
Pros: quiet, travel-friendly, no mask or hose.
Cons/side effects: jaw soreness, tooth discomfort, bite changes over time, possible TMJ aggravation; dental fitting/monitoring and follow-up testing are important. Sources: SleepApnea.org (2025); PMC reviews
Candidate pointers: consider AHI range, symptoms, dental health, jaw/TMJ history, and positional patterns.
Conclusion: Oral appliances can be highly effective for the right patient—confirm results with testing.

2) Advanced PAP Options (If Standard CPAP Is the Problem—Not PAP Itself)
APAP automatically adjusts pressure through the night and may feel easier than fixed settings, especially when needs vary by stage or position. Source: Sleep Foundation (2025)
BiPAP uses different pressures for inhale and exhale to reduce the breathing against the machine sensation for some patients. Source: Sleep Foundation (2025)
EPAP devices are small and create resistance during exhalation; useful in select cases with careful selection. Source: Sleep Foundation (2025)
Who should consider: those with pressure intolerance, aerophagia, or comfort issues—guided by clinical data. Source: Sleep Foundation (2025)
Conclusion: If PAP works clinically but not comfortably, switching modes can be the easiest fix.

3) Positional Therapy (When Your Apnea Is Worse on Your Back)
Signs of positional OSA: a sleep study shows far more events when supine, turning snoring-on-my-back into an actionable plan.
Usable options: side-sleep training, wearable vibratory prompts, and other positioning tools. Sources: SleepApnea.org (2025); Sleep Foundation (2025)
Combining therapies: often paired with an oral appliance or weight management for additive effect. Sources: SleepApnea.org (2025); Sleep Foundation (2025)
Conclusion: If your apnea is posture-sensitive, avoiding back-sleep can meaningfully reduce events.
4) Myofunctional Therapy (Targeted Mouth/Throat Exercises)
What it is: structured exercises targeting tongue, soft palate, and facial muscles; more like physical therapy than a quick fix.
Best for: mild OSA/snoring, mouth-breathing patterns, or as an add-on. Source: Sleep Foundation (2025)
Evidence: can reduce OSA severity for some and improve symptoms, especially with strong adherence. Source: PMC12561462
Conclusion: A helpful adjunct—especially when you’ll stick with it.

5) Weight Management (One of the Highest-Impact Options for Many Patients)
Why weight matters: body weight influences airway size and collapsibility; improvements in weight often correlate with OSA improvements. Sources: Sleep Foundation (2025); Harvard Health (2020)
Realistic improvements: reduced AHI and symptoms; sometimes remission—verify with repeat testing. Sources: Sleep Foundation (2025); Harvard Health (2020)
Bariatric surgery: can substantially reduce severity in qualifying patients, but OSA may persist; long-term follow-up is key. Source: Harvard Health (2020)
Practical plan: medical weight management, nutrition, activity, consistent sleep schedules—often alongside another therapy. Source: Sleep Foundation (2025)
Conclusion: Weight-focused approaches can be powerful—verify improvement with repeat testing and monitor over time.
6) Medications (New in 2025: Zepbound for Sleep Apnea)
Zepbound became the first medication approved specifically for sleep apnea in qualifying patients—working primarily through weight loss and reducing breathing disruptions. Source: Sleep Foundation (2025)
Who may benefit: patients with OSA and obesity under individualized medical criteria and monitoring. Source: Sleep Foundation (2025)
Cautions: not a substitute for diagnosis or follow-up testing; monitor side effects and contraindications. It targets weight-related drivers and is not a standalone fix for airway collapse. Source: Sleep Foundation (2025)
Other meds: some address residual sleepiness (a symptom) rather than airway obstruction. Source: Sleep Foundation (2025)
Conclusion: Medication can support weight-related drivers of OSA, but it doesn’t replace airway-targeted treatment or testing.
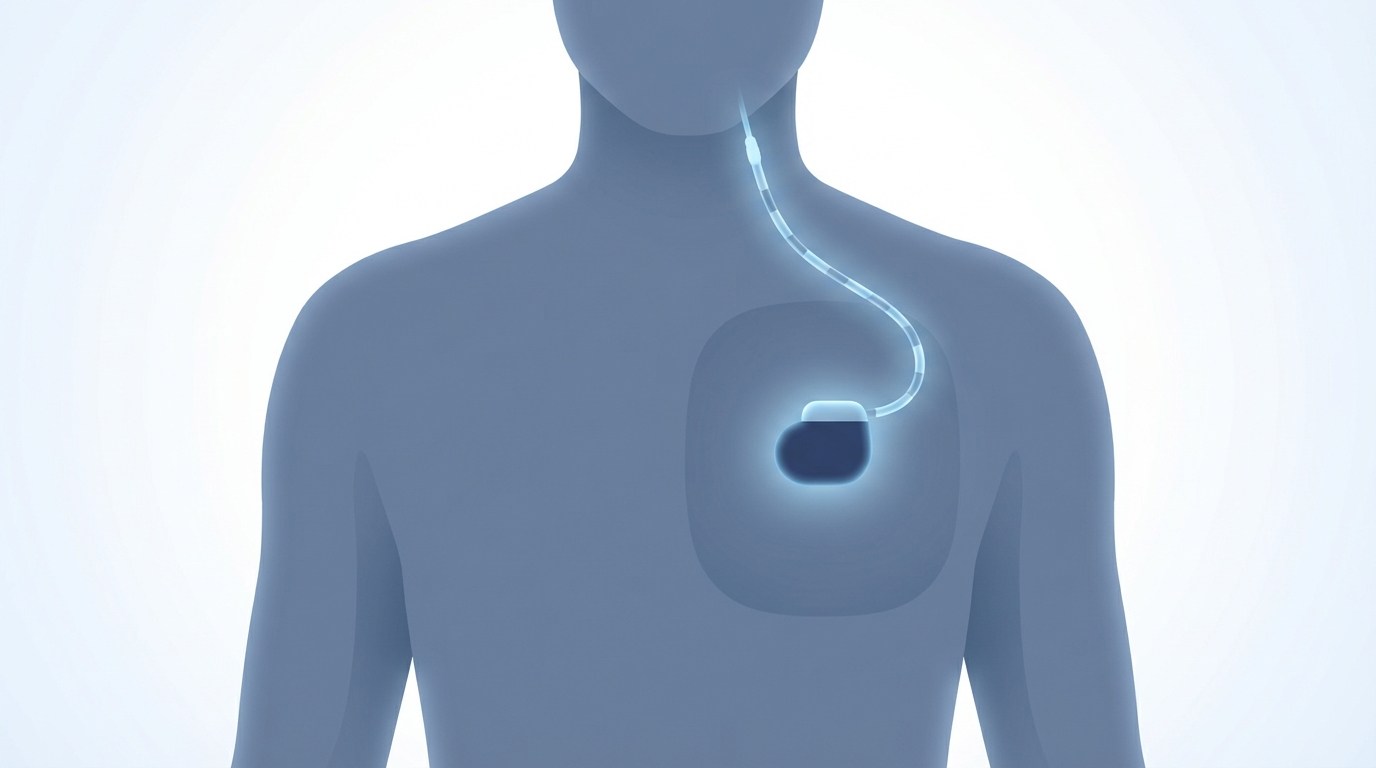
7) Implantable Therapy: Hypoglossal Nerve Stimulation (Inspire)
How it works: stimulates the hypoglossal nerve to activate tongue muscles and help keep the airway open. Sources: SleepApnea.org (2025); Sleep Foundation (2025)
Common selection factors: moderate to severe OSA, CPAP failure or intolerance, and specific airway findings. Source: SleepApnea.org (2025)
Evaluation: updated sleep testing and airway assessment; some undergo DISE (drug-induced sleep endoscopy). Source: SleepApnea.org (2025)
Pros: no mask/hose, often well-tolerated. Cons: requires a procedure and device management; not everyone qualifies.
Conclusion: A strong option for selected patients who can’t tolerate CPAP and meet eligibility criteria.
8) Surgery for Sleep Apnea (When Anatomy Is the Main Driver)
Approaches: nasal surgery, tonsil/adenoid surgery when relevant, palate procedures, or jaw surgery in select cases. Sources: Harvard Health (2020); Sleep Foundation (2025)
What to expect: surgery can reduce obstruction, but outcomes vary; some still need additional therapies afterward. Sources: Harvard Health (2020); Sleep Foundation (2025)
Planning: set realistic goals, understand recovery, and arrange repeat sleep testing. Source: Sleep Foundation (2025)
Conclusion: Surgery can be impactful for the right anatomy—plan on follow-up testing and possible combination therapy.
“What About…?” Common Non-CPAP Products (And the Evidence Reality Check)
Nasal strips and dilators
May improve nasal airflow and reduce snoring for some, but usually insufficient for true OSA. Source: SleepApnea.org (2025)
Mouth tape
Not a primary OSA treatment and may pose risks if nasal breathing is limited; use only with medical advice. Source: SleepApnea.org (2025)
Supplements and herbal remedies
Evidence is limited; they don’t replace therapies shown to reduce apnea events. Source: SleepApnea.org (2025)
Conclusion: Helpful add-ons can’t replace treatments proven to keep your airway open.
How to Choose the Right CPAP Alternative (Step-by-Step)
Step 1—Confirm severity and type
Use AHI, oxygen data, and symptoms to guide decisions. Source: Sleep Foundation (2025)
Step 2—Match treatment to your pattern
- Positional OSA → positional therapy
- Mild–moderate OSA → oral appliance often reasonable
- Moderate–severe with CPAP intolerance → consider implant/surgery pathways
- Obesity-related OSA → weight management and, when appropriate, medication such as Zepbound
Sources: Sleep Foundation (2025); SleepApnea.org (2025)
Step 3—Confirm results
Confirm effectiveness with repeat sleep testing or device data plus symptom tracking (quieter nights, better mornings, and improved numbers). Source: Sleep Foundation (2025)
Conclusion: Choose based on your data, and always verify that your treatment works.
Lifestyle Tips That Make Any Treatment Work Better
- Alcohol timing and sedatives: these can worsen airway collapse for some.
- Sleep position: even small positioning changes can matter in positional OSA.
- Nasal breathing support: manage allergies/rhinitis and congestion to improve comfort.
- Consistency and follow-up: adherence often beats the perfect option that doesn’t get used.
Conclusion: Small daily habits can amplify the impact of any therapy you choose.
FAQs About CPAP Alternatives
What is the best alternative to CPAP for sleep apnea?
It depends on severity, anatomy, and sleep study findings. Common options include oral appliances, APAP/BiPAP, weight-focused strategies, Inspire, and selected surgeries. CPAP remains the frontline standard for most who can tolerate it. Sources: Sleep Foundation (2025); SleepApnea.org (2025)
Do oral appliances work as well as CPAP?
CPAP often reduces AHI more strongly in ideal conditions, but oral appliances can be highly effective for selected patients—and real-world adherence can be higher for some. Sources: PMC reviews; SleepApnea.org (2025)
Can weight loss cure sleep apnea?
Weight loss can significantly reduce severity and sometimes lead to remission, but follow-up testing is important because OSA may persist. Sources: Harvard Health (2020); Sleep Foundation (2025)
Is Inspire better than CPAP?
It isn’t a simple better/worse comparison. Inspire may be a strong option for those who meet criteria and cannot tolerate CPAP, while CPAP remains highly effective and broadly applicable as first-line when tolerated. Sources: SleepApnea.org (2025); Sleep Foundation (2025)
Can I combine treatments (like MAD + positional therapy)?
Yes—combination therapy is common, especially for mild to moderate OSA or positional patterns. Sources: Sleep Foundation (2025); SleepApnea.org (2025)
How do I know if my alternative is working?
Track symptom changes (snoring, sleepiness, headaches) and confirm with repeat testing or device data. Source: Sleep Foundation (2025)
Conclusion: The best alternative is the one you’ll use consistently—and that follow-up data confirms is effective.
Conclusion—A Better Night’s Sleep Is Possible Without White-Knuckling CPAP
Proven CPAP alternatives exist, including oral appliances, advanced PAP options (APAP/BiPAP/EPAP), weight management (including newer medications), positional and myofunctional therapy, Inspire, and surgery—each with different strengths depending on your diagnosis. CPAP remains the standard first-line therapy when tolerated, but if it isn’t working for you, there are validated paths forward.
If you’re exploring options, Sleep and Sinus Centers of Georgia can help you understand your testing results, compare treatments, and arrange follow-up to confirm what’s working. Book an appointment: https://sleepandsinuscenters.com/ Learn more: https://sleepandsinuscenters.com/snoring-sleep-apnea-treatment
Conclusion: You don’t have to choose between poor sleep and an intolerable mask—there is a data-backed path to better nights.
Sources and Disclaimer
Sources used: Sleep Foundation (2025) https://www.sleepfoundation.org/sleep-apnea/alternatives-to-cpap ; SleepApnea.org (2025) https://www.sleepapnea.org/treatment/alternatives-to-cpap/ ; Harvard Health (2020) https://www.health.harvard.edu/staying-healthy/beyond-cpap-other-options-for-sleep-apnea ; PMC evidence summaries https://pmc.ncbi.nlm.nih.gov/articles/PMC10684110/ , https://pmc.ncbi.nlm.nih.gov/articles/PMC9584565/ , https://pmc.ncbi.nlm.nih.gov/articles/PMC12561462/
Disclaimer: This article is for educational purposes only and is not medical advice. Consult a qualified healthcare provider for diagnosis and treatment.
Don’t let allergies slow you down. Schedule a comprehensive ENT and allergy evaluation at Sleep and Sinus Centers of Georgia. We’re here to find your triggers and guide you toward lasting relief.








