Chronic Sinusitis Not Caused by Allergies or Infection: Common Non-Allergic Causes and Treatment Options
If your sinus symptoms keep coming back—but allergy tests are negative and antibiotics don’t help—you’re not imagining it. Chronic sinusitis not caused by allergies or infection is common, and it often has very real (and treatable) underlying drivers.
This article breaks down the most frequent non-allergic, non-infectious reasons people develop long-lasting sinus symptoms, how an ENT specialist evaluates them, and the treatment options that may help. Importantly, several triggers can overlap at the same time—like structural blockage plus irritant exposure plus reflux—so identifying your main contributors is key. Sources including the Merck Manual, Cedars-Sinai, Medscape, and AAFP recognize these non-infectious pathways for persistent sinus inflammation. [1–5]
For a broader foundation, you can also review our chronic sinusitis overview: https://sleepandsinuscenters.com/chronic-sinusitis
What Counts as "Chronic Sinusitis" (and Why It Can Happen Without Allergy or Infection)
Definition and timeline
Chronic sinusitis (often discussed clinically as chronic rhinosinusitis) generally means sinus-related symptoms lasting 12 weeks or longer. [5] This timeframe matters because ongoing symptoms are more likely to reflect persistent inflammation, anatomy/drainage issues, or irritant sensitivity, rather than a short-lived infection.
A helpful way to think about it: an acute infection is like a storm that passes. Chronic symptoms are more like a drainage system that keeps clogging—even when there’s no “new storm” (no active infection) and no clear allergy trigger.
Sinusitis vs. rhinitis—why it’s confusing
Sinus symptoms and nasal symptoms overlap. Rhinitis is inflammation of the nasal lining, while sinusitis involves inflammation of the sinus cavities. But congestion, postnasal drip, and facial pressure can show up in either condition—and they can occur without bacterial infection. [1–2]
It’s also common to have both at the same time. An ENT might explain it like this: “Your nose is the hallway. Your sinuses are the side rooms. If the hallway stays swollen, the side rooms don’t ventilate well.”
If you’ve been told you might have “nonallergic rhinitis,” our page on treating chronic rhinitis explains how nasal inflammation can mimic sinus problems: https://sleepandsinuscenters.com/treating-chronic-rhinitis
Bottom line: chronic symptoms often reflect ongoing inflammation and drainage problems—not just allergy or infection.
Common Symptoms of Chronic Sinusitis (Even When It’s Not Allergies or Infection)
Core symptoms patients notice
- Nasal congestion or blockage
- Facial pressure/fullness
- Thick drainage or postnasal drip
- Reduced sense of smell/taste [1]
These symptoms can still occur without active infection, especially when inflammation and drainage problems persist. In real life, this might look like being “always stuffed up,” needing to mouth-breathe at night, or feeling pressure when you bend forward—even without fever.
“Silent” or less obvious symptoms
- Headache that doesn’t clearly match imaging findings
- Bad breath
- Chronic cough or throat clearing
- Fatigue or poor sleep related to nasal obstruction [1]
For example, some people come in thinking they have a lingering cold, but what’s really happening is night-after-night mouth breathing, fragmented sleep, and throat irritation from constant drainage.
When symptoms suggest something else
Some symptoms are considered red flags and should be evaluated urgently, such as high fever, swelling around the eyes, severe one-sided symptoms, or neurological symptoms. [1] Seek urgent medical attention if any of these occur.
In short: if symptoms last more than 12 weeks—or include red flags—get evaluated rather than assuming it’s “just another cold.”
Why Chronic Sinusitis Happens Without Allergies or Infection (Non-Allergic Causes)
Overlap is common
Many people don’t have just one cause. It’s common for structural narrowing + irritant exposure + reflux (or other factors) to stack together—making symptoms persistent until the full picture is addressed.
Structural and anatomic causes (drainage gets blocked)
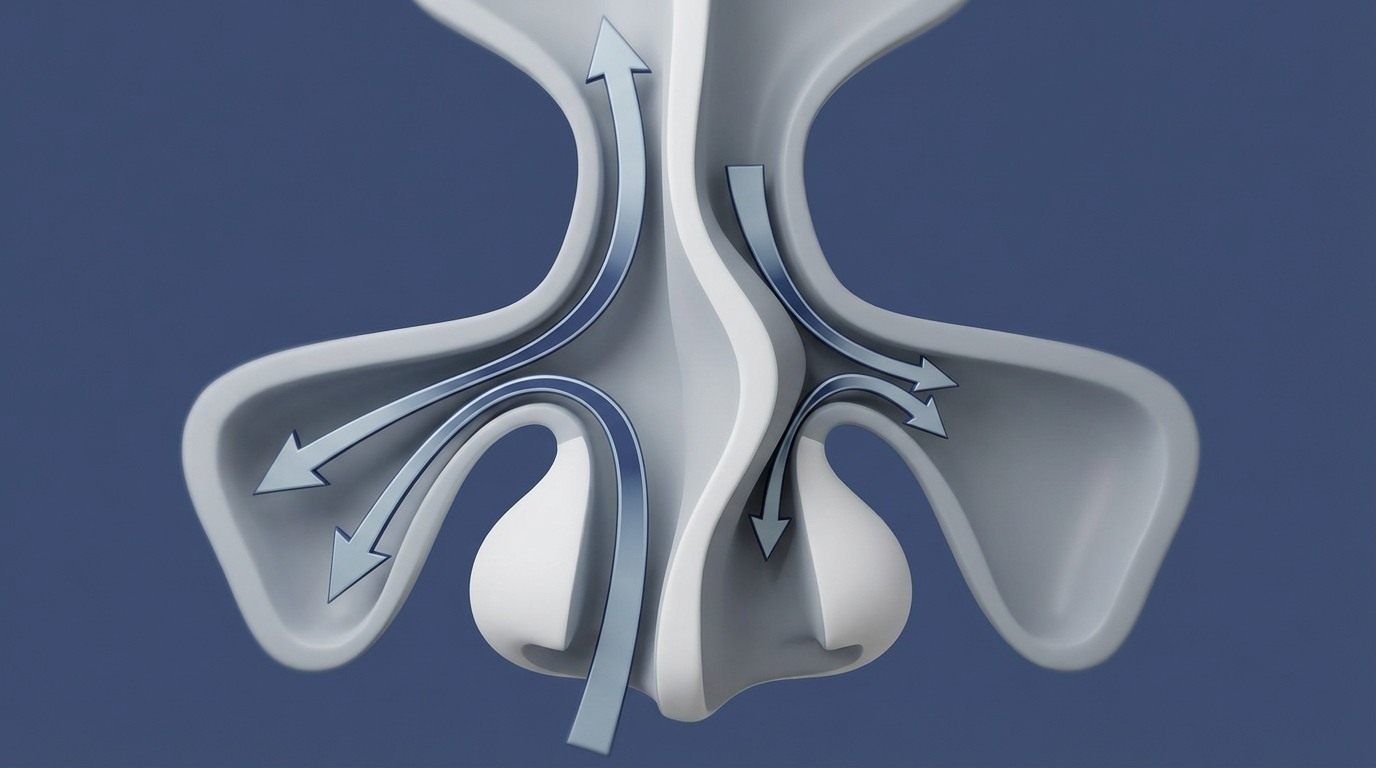
When the nasal/sinus passages don’t ventilate and drain well, inflammation can linger. Common structural contributors include:
- Deviated septum
- Nasal polyps
- Turbinate enlargement or naturally narrow drainage pathways [1,4]
Why it matters: your sinuses constantly produce mucus. If the “exit pathways” are narrow or swollen, mucus doesn’t clear well—like a sink that drains slowly. The result can be ongoing congestion, pressure, and thick postnasal drip, even without an active infection. That’s one reason chronic symptoms may persist despite standard allergy or infection treatments. [1,4]
Environmental irritants (non-allergic inflammation triggers)
Even without allergies, the nasal lining can react strongly to irritants such as:
- Tobacco smoke (including secondhand exposure)
- Air pollution/smog/particulates
- Strong odors, fragrances, cleaning chemicals, and occupational exposures [1–2]
These exposures are well-recognized nonallergic sinusitis causes, and reducing them can be a major part of symptom control. [1–2] Practically, this might mean symptoms flaring after cleaning with strong sprays, being around cigarette smoke, working in dusty environments, or even walking through heavy perfume.

Systemic or “whole-body” contributors
Some drivers aren’t local to the nose—they affect inflammation, mucus, or immune function throughout the body. Examples include:
- Immunodeficiency, which can contribute to recurrent or persistent inflammation
- Impaired ciliary function (reduced ability to move mucus)
- Genetic conditions such as cystic fibrosis
- Aspirin-Exacerbated Respiratory Disease (AERD), often associated with nasal polyps
- Gastroesophageal reflux disease (GERD) and laryngopharyngeal reflux (LPR), which may irritate the upper airway and worsen nasal symptoms [1,3–4]
These are important to consider when evaluating chronic sinus inflammation causes, especially when symptoms recur despite usual treatments. [1,3–4] Conditions such as immunodeficiency, cystic fibrosis, and suspected ciliary disorders typically require specialist evaluation.
Medication-related causes (including rebound congestion)
Certain medications can worsen dryness, congestion, or nasal lining irritation. Also, overuse of topical decongestant sprays can cause rebound congestion—a cycle where the nose feels increasingly blocked as the spray wears off. [1–2]
If this sounds familiar, see our related resource on rebound congestion from Afrin: https://sleepandsinuscenters.com/blog/afrin-rebound-how-long-does-nasal-congestion-last-after-use
Hormones, diet, and nervous system triggers
Not all congestion is allergic—and not all triggers are obvious. Some people notice symptoms worsen with:
- Hormonal shifts (including pregnancy or thyroid disease)
- Alcohol or spicy foods (sometimes called “gustatory” effects)
- Stress and poor sleep, which may amplify nasal reactivity [2–3]
A simple experiment is to track symptoms for a couple of weeks and look for consistent patterns—like congestion after late meals (possible reflux clue) or a runny nose after spicy food.
In summary: multiple nonallergic factors can drive persistent symptoms, and several often overlap.
How Doctors Figure Out the Cause (So Treatment Actually Works)
Key history questions that change the diagnosis
A targeted history often reveals patterns that point away from infection and toward specific nonallergic drivers, such as:
- Did antibiotics help, or not at all?
- What did allergy testing show?
- Do symptoms flare with smoke, perfume, weather changes, or certain meals (reflux clues)?
- Is obstruction one-sided or both sides? Is it constant or variable?
This is particularly relevant when you suspect chronic sinusitis not caused by allergies or infection, because the “why” determines the next step. For instance, constant one-sided blockage may raise concern for a structural issue, while “fine at home, awful at work” can suggest an irritant exposure pattern.
Physical exam + nasal endoscopy
ENT clinicians often use a detailed nasal exam and may perform nasal endoscopy to look for swelling, drainage, polyps, and structural blockage. [4–5] Patients often describe endoscopy as “weird but quick.” It’s useful because it lets your doctor see what a mirror can’t—especially deeper swelling, polyps, or mucus patterns that suggest poor drainage.
When imaging helps (CT scan)
A CT scan can help confirm chronic inflammation patterns, identify anatomic narrowing, and support surgical planning when needed. [4–5] It’s not always the first step, but it can be clarifying when symptoms persist and the cause isn’t obvious from exam alone.
Bottom line: a focused history, in-office exam with endoscopy, and selective imaging help pinpoint the true drivers of your symptoms.

Treatment Options for Non-Allergic (Non-Infectious) Chronic Sinusitis
Because multiple factors can contribute, treatment plans often combine approaches. The options below are commonly used in persistent inflammatory sinus conditions. Individual plans may vary and should be guided by a clinician. [1,5]
First-line home care (foundation for most patients)
Many care plans start with “foundation” steps that support mucus clearance and moisture, such as:
- Saline irrigation (often used regularly to flush irritants and thin mucus) [1,5]
- Humidification strategies when dry air worsens symptoms
- Hydration and nasal moisture support
Irrigation is like rinsing pollen, dust, or smoke residue off your skin after being outdoors—except you’re doing it for the nasal lining. Technique and frequency vary by person; many patients do best after getting clear instructions from their clinician.

Medications commonly used (even when it’s not allergy or infection)
Even without active infection, anti-inflammatory therapy may be used to calm swelling and improve drainage, including:
- Intranasal corticosteroid sprays (not only for allergies; often used for inflammation control) [5]
- Anticholinergic nasal spray when runny nose is prominent (a common nonallergic rhinitis pattern) [2,5]
- Select short-term oral medications in specific situations, based on clinician assessment (avoid self-medicating with antibiotics or oral steroids; these are not routinely indicated without evidence of infection) [2,5]
The goal is to reduce swelling so the drainage pathways reopen—rather than trying to “kill bacteria” when bacteria aren’t the main problem.
Addressing irritants and triggers (environment-focused care plan)
Reducing exposure can meaningfully improve symptoms for people with nonallergic sinusitis causes. Common strategies include:
- Smoke cessation and minimizing secondhand smoke exposure [1–2]
- Fragrance-free and low-irritant cleaning routines
- Workplace exposure mitigation when occupational triggers are involved [1–2]
For practical ideas, see avoiding irritants that trigger sinus flare-ups: https://sleepandsinuscenters.com/blog/avoiding-irritants-that-trigger-sinus-flare-ups
Treating reflux-driven sinus symptoms (when GERD/LPR is suspected)
When reflux is part of the picture, clinicians may discuss lifestyle patterns (like timing of meals and late-night eating), positional strategies, and medications as appropriate. Reflux can be a meaningful contributor to chronic sinusitis not caused by allergies or infection in some patients. [1,4]
A common clue is symptoms that worsen at night or in the morning—especially when paired with throat clearing, hoarseness, or a sour taste.

Correcting “rebound congestion” from decongestant sprays
If rebound congestion is suspected, the plan often involves a supervised taper and shifting toward saline support and anti-inflammatory therapies. [1–2] This is a common reason “nothing seems to work,” even when there’s no infection—because the nose is reacting to the medication cycle itself.
When procedures or surgery may help
When persistent symptoms are driven by obstruction or anatomy—and medical therapy hasn’t been enough—procedures may be considered, such as:
- Balloon sinuplasty for selected blockage patterns
- Endoscopic sinus surgery for ongoing obstruction/polyps despite appropriate medical therapy
- Septoplasty/turbinate reduction when anatomy is the main barrier [4–5]
If you’re exploring procedure options, learn more about Balloon Sinuplasty: https://sleepandsinuscenters.com/balloon-sinuplasty
Key takeaway: combining moisture, inflammation control, trigger reduction, and—when appropriate—procedures tends to deliver the best results.
Lifestyle Tips to Reduce Flare-Ups (Patient-Friendly Checklist)
Home and air quality habits
- Use HEPA filtration when helpful; maintain HVAC filters; improve ventilation
- Reduce fragrances; avoid burning candles/incense if they trigger symptoms
Daily “sinus-friendly” routine
- Keep a consistent rinse schedule if it helps you
- Shower and change clothes after heavy outdoor pollutant exposure when feasible
Food, alcohol, and hydration
- Consider tracking symptoms after alcohol or spicy foods to see if they’re triggers
- Hydration needs vary; some people notice dryness worsens congestion, while others are more sensitive to caffeine—individual patterns matter
Simple, consistent habits can reduce the frequency and intensity of flares.
FAQs (Optimized for Featured Snippets)
Can you have chronic sinusitis with negative allergy tests?
Yes. Irritants, structural blockage, reflux, and immune-related factors can all drive persistent inflammation even when allergy testing is negative. [1–2]
Why don’t antibiotics fix my chronic sinus symptoms?
Chronic symptoms are often more inflammatory or structural than bacterial, so antibiotics may not address the underlying problem in many cases. [5]
What’s the difference between nonallergic rhinitis and chronic sinusitis?
Rhinitis is inflammation of the nasal lining; sinusitis involves inflammation of the sinuses. Symptoms overlap, and many people have both patterns at the same time. [1–2] More on overlap: treating chronic rhinitis: https://sleepandsinuscenters.com/treating-chronic-rhinitis
How do I know if I have nasal polyps?
Polyps are usually identified through symptoms plus an in-office exam and often nasal endoscopy; imaging can also help in some cases. [4–5]
When should I see an ENT for chronic sinus symptoms?
Consider evaluation when symptoms last longer than 12 weeks, keep recurring, don’t respond to reasonable OTC measures, cause significant obstruction, or include red-flag symptoms. [1,5]
Conclusion + Next Step
Chronic sinusitis not caused by allergies or infection is real—and often very manageable once the main driver (or combination of drivers) is identified. Structural narrowing, irritant exposure, reflux, medication effects, and systemic conditions can all contribute to persistent symptoms. [1–5]
If symptoms have lingered for months or keep returning despite typical allergy or antibiotic approaches, an ENT evaluation can help clarify what’s actually fueling the inflammation. Diagnosis and treatment require medical evaluation.
Ready for answers? Book an appointment with Sleep and Sinus Centers of Georgia: https://www.sleepandsinuscenters.com/
Medical disclaimer: This article is for general education and is not a substitute for personalized medical advice, diagnosis, or treatment.
This article is for educational purposes only and is not medical advice. Please consult a qualified healthcare provider for diagnosis and treatment.
Sources
1. Merck Manual Consumer Version – Sinusitis: https://www.merckmanuals.com/home/ear-nose-and-throat-disorders/nose-and-sinus-disorders/sinusitis
2. Cedars-Sinai – Nonallergic Sinusitis: https://www.cedars-sinai.org/health-library/diseases-and-conditions/n/nonallergic-sinusitis.html
3. NCBI Bookshelf – Sinusitis overview: https://www.ncbi.nlm.nih.gov/books/NBK441934/
4. Medscape – Sinusitis overview: https://emedicine.medscape.com/article/232791-overview
5. AAFP – Chronic Rhinosinusitis guidance: https://www.aafp.org/pubs/afp/issues/2018/0801/p171.html
Don’t let allergies slow you down. Schedule a comprehensive ENT and allergy evaluation at Sleep and Sinus Centers of Georgia. We’re here to find your triggers and guide you toward lasting relief.








