Can Turbinates Grow Back After Turbinate Reduction?
If you’ve had (or are considering) turbinate reduction, it’s natural to wonder what happens long-term—especially if congestion starts creeping back in. The reassuring news is that when symptoms return, it often reflects ongoing inflammation—such as allergies or chronic rhinitis—rather than a failure of the procedure.
A helpful way to think about it: turbinate tissue is a responsive “air filter,” not a rigid wall. Even after reduction, the remaining tissue can still react to triggers—sometimes quietly, sometimes dramatically.
Below, we’ll break down what “regrowth” really means, why it happens, what’s normal during healing, and how an ENT specialist evaluates and manages recurrent nasal obstruction.
Quick Answer: Can Turbinates Grow Back After Turbinate Reduction?
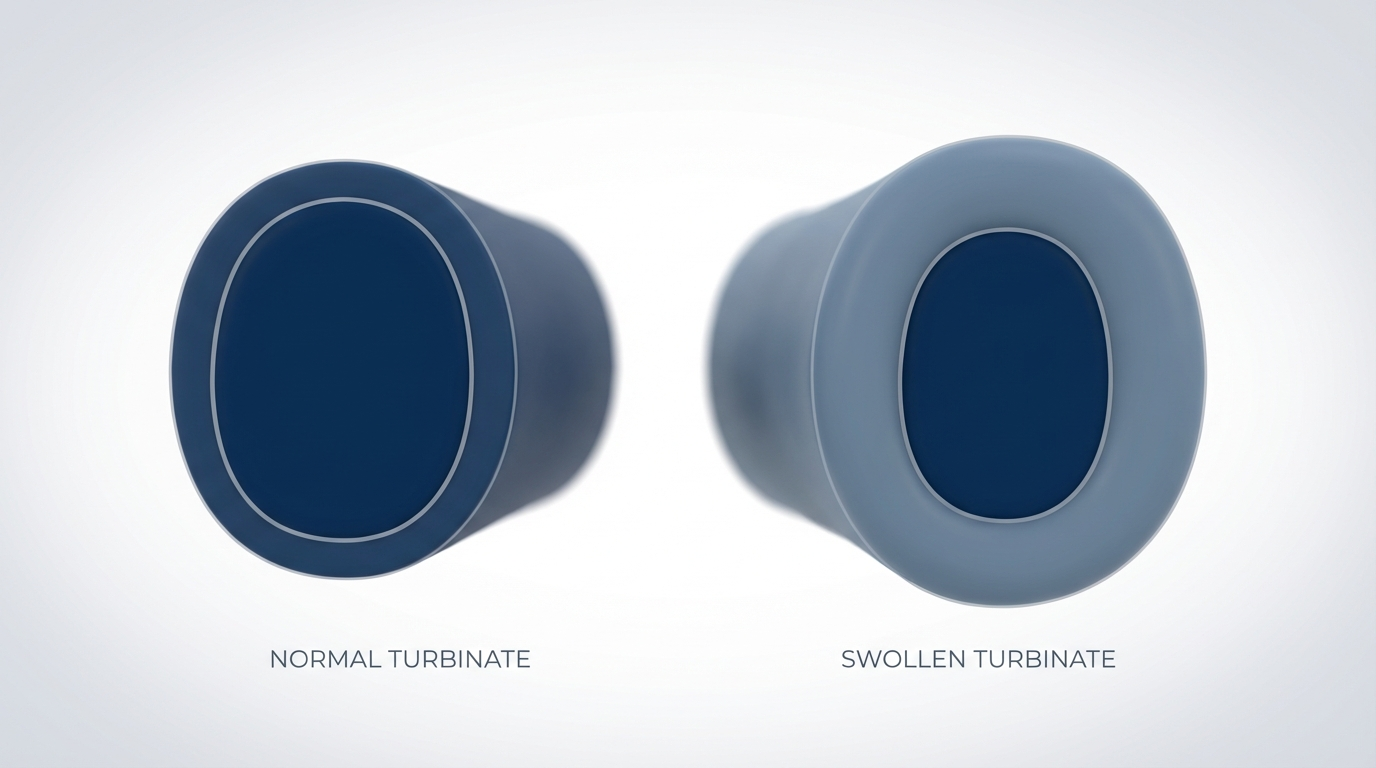
While true tissue regrowth after turbinate reduction is uncommon, the remaining turbinate tissue can swell significantly over time—often due to allergies, irritants, or chronic rhinitis—which can make symptoms feel like they “came back.” Some limited structural changes may occur, but symptom recurrence is primarily due to mucosal swelling rather than significant new tissue growth (see an overview from the Cleveland Clinic: https://my.clevelandclinic.org/health/treatments/22805-turbinate-reduction).
- If you’re exploring the procedure itself, see our guide: Everything You Need to Know About Turbinate Reduction: https://sleepandsinuscenters.com/blog/everything-you-need-to-know-about-turbinate-reduction
Bottom line: most post-surgery “return of congestion” is driven by swelling of the remaining lining, not true regrowth.
What Are Turbinates and Why Do They Get Enlarged?
What turbinates do (warming, humidifying, filtering air)
Turbinates are curved structures inside the nose covered with soft tissue. They help warm and humidify the air you breathe, filter particles and irritants, and direct airflow through the nasal passages. Because the lining is responsive tissue, it can swell when your nose is irritated or inflamed. Even mild swelling inside a narrow airway can feel “huge.”
Turbinate hypertrophy explained (chronic swelling)
Turbinate hypertrophy means the turbinate tissue is persistently enlarged—often due to ongoing inflammation. This can reduce airflow and create the sensation of “always being congested,” even without a cold.
Common conditions linked to enlarged turbinates
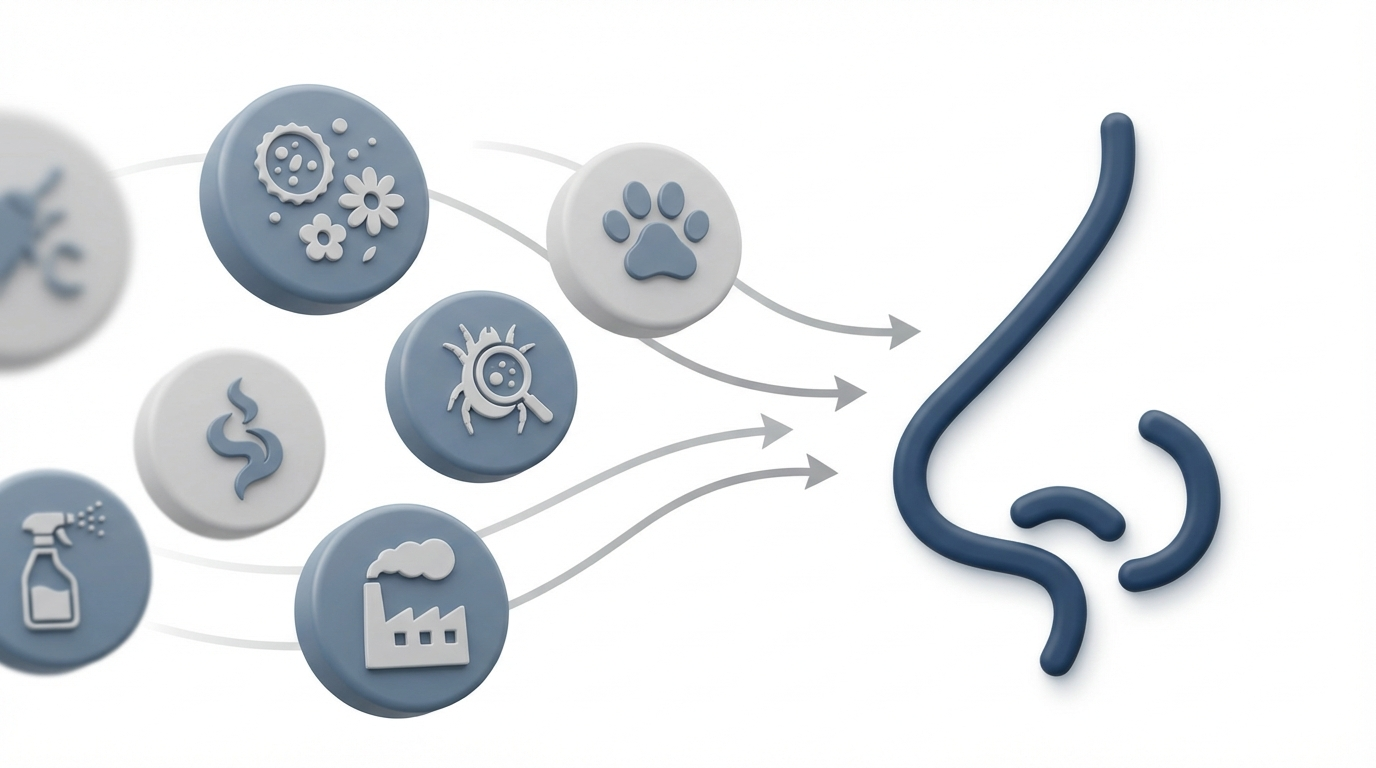
- Allergic rhinitis (seasonal or year-round allergies)
- Nonallergic rhinitis (irritants like smoke, strong odors, or weather changes)
- Chronic sinus inflammation
- Structural issues, such as a deviated septum, that can worsen the sensation of blockage
For a deeper dive into one common approach, read about inferior turbinate reduction: https://sleepandsinuscenters.com/blog/inferior-turbinate-reduction-breathe-easier-without-the-or
Turbinates are meant to respond to your environment—so inflammation and irritants often drive the feeling of “blocked again.”
Why Turbinates Can “Come Back” After Surgery (The Real Reasons)
Ongoing allergies or irritant exposure (most common driver)
The biggest reason symptoms return is continued inflammation. Even after turbinate reduction, the remaining lining can still react to triggers such as pollen, dust mites, mold, pet dander, smoke or vaping aerosols, strong fragrances or cleaning chemicals, and pollution. If rhinitis remains active, turbinates can swell again over time—sometimes gradually, sometimes seasonally. Learn more: https://sleepandsinuscenters.com/treating-chronic-rhinitis
Surgical technique and how much tissue was preserved
Modern techniques aim to improve airflow while preserving function—warming, humidifying, and filtering air—because turbinates are key to healthy nasal breathing (overview: https://my.clevelandclinic.org/health/treatments/22805-turbinate-reduction).
Individual healing response (scarring vs swelling patterns)
Healing varies. Some people experience more prolonged internal swelling, crusting or dryness, and different patterns of tissue remodeling. These differences influence how the nose feels during recovery and months later.
Time-related return of symptoms
Even with a well-performed procedure, symptoms can return if underlying drivers aren’t controlled. Many enjoy long-lasting relief, but durability depends on inflammation control, exposures, and anatomy.
If symptoms return, inflammation is usually the culprit—not significant new turbinate tissue growth.
Symptoms That May Suggest Turbinate Swelling or Recurrence
Breathing and congestion symptoms
- Nasal blockage on one side or both
- Feeling like you “can’t breathe through your nose at night”
- Mouth breathing and waking with a dry mouth
Sleep and quality-of-life symptoms
- Snoring that worsens over time
- Poor sleep quality or waking up unrefreshed
Irritation and drainage symptoms
- Postnasal drip, runny nose (especially with triggers), and facial pressure (sometimes)
A calming reminder: in the early healing phase after surgery, congestion is very common due to swelling and crusting and is not necessarily recurrence. If congestion persists or worsens beyond the early healing period, it’s worth an evaluation.

Normal Healing vs Recurrence: What’s Expected After Turbinate Reduction?
Early post-op congestion can be normal
After a turbinate reduction, it’s common to experience temporary swelling, crusting, dryness, and fluctuating congestion. Airflow typically improves as swelling settles (post-op expectations: https://my.clevelandclinic.org/health/treatments/22805-turbinate-reduction).
When improvement typically starts
Some notice airflow improvement relatively quickly, while others feel gradual change over several weeks. Day-to-day variability is common.
Signs it may be more than normal healing
- Symptoms improve, then return months or years later
- Congestion is strongly linked with season changes, pet exposure, or dusty environments
- Nasal blockage becomes persistent again despite the initial benefit
Note: persistent or worsening congestion after several weeks should prompt evaluation by an ENT specialist. Short-term ups and downs are part of healing; persistent or worsening symptoms deserve a closer look.

How ENT Specialists Check for Turbinate Swelling or Other Causes
Nasal exam and symptom history
Evaluation starts with your symptom timeline, triggers, and response to prior treatments. Practical details matter—such as whether symptoms spike after cleaning, travel, yard work, or sleeping with a fan or humidifier.
Nasal endoscopy (quick in-office look)
An ENT specialist may use nasal endoscopy to assess turbinate size and swelling, septum alignment, and signs of inflammation, mucus, or polyps.
Allergy evaluation if inflammation is suspected
If symptoms are seasonal, trigger-based, or persistent, allergy testing may help identify drivers: https://sleepandsinuscenters.com/allergy-testing
Rule out other causes of obstruction
Not all “post-turbinate” congestion is turbinate-related. An ENT may also consider deviated septum, nasal valve collapse, nasal polyps, or chronic sinusitis.
A thorough evaluation can distinguish true recurrence from other common causes of nasal blockage.

Treatment Options If Turbinates Swell Again
Medical treatments (often first-line)
When inflammation drives symptoms, non-surgical options are often considered first. Depending on the situation, treatment categories may include nasal steroid sprays (to reduce inflammation over time), antihistamines (when allergy-driven symptoms are present), saline irrigation (to rinse irritants and mucus), and avoiding frequent use of topical decongestant sprays that can cause rebound congestion when overused.
Allergy management to protect surgery results
Because inflammation is a common root cause, allergy care can help maintain results. Strategies may include environmental controls and, when appropriate, immunotherapy—tailored to the individual.
Office-based procedures (if appropriate)
In select cases, minimally invasive, office-based options may help reduce recurrent swelling.
Revision turbinate surgery (less common)
When symptoms are significant and conservative options haven’t helped, revision surgery may be considered. A key goal is balancing airflow improvement with preservation of turbinate function.
Most people do well with medical and environmental strategies; procedures are tailored when symptoms persist.
Lifestyle Tips to Help Prevent Turbinate Swelling After Surgery
Allergen and irritant reduction at home
- HEPA filtration
- Allergen-proof bedding covers
- Maintain indoor humidity within a comfortable range
- Avoid smoke exposure
Daily nasal care routines
- Saline sprays or rinses (as tolerated)
- Good hydration
- Use a humidifier when air is dry
Seasonal action plan
If you have predictable seasonal symptoms, plan ahead with your clinician. Start your allergy routine before peak pollen season rather than waiting until congestion is severe.
Medication adherence and follow-up care
Following post-op instructions and attending follow-up visits help ensure healing is on track and inflammation is addressed early if it returns.
Small, consistent habits often make the biggest difference over time.
When to Call Your ENT Specialist (Red Flags)
Symptoms that need evaluation—do not delay
- Persistent nasal obstruction that is worsening
- Frequent nosebleeds or severe dryness/crusting
- Concerning pain or swelling
- Recurrent infections or facial swelling
If symptoms return after a period of improvement
If congestion noticeably returns after an initial period of relief, it may signal that inflammation needs better control or that another nasal issue is contributing.
Timely evaluation helps identify the cause and keeps your recovery on track.
FAQs — Can Turbinates Grow Back After Turbinate Reduction?
How common is turbinate “regrowth” or swelling?
It varies. In many cases, what people experience is recurrent swelling tied to allergies, irritants, or chronic rhinitis—not true regrowth.
How long does turbinate reduction last?
Results vary widely. Many people experience long-lasting relief, while others notice symptoms gradually returning if triggers persist.
Is it regrowth of bone or soft tissue?
Most recurrence relates to swelling of the soft tissue lining (mucosa). Significant new bone growth is not typically the main cause of symptoms.
Can allergies undo the results of turbinate reduction?
Allergies can contribute to renewed inflammation and swelling, which may make it feel like the benefits faded. Controlling allergic rhinitis often supports longer-lasting comfort (overview: https://my.clevelandclinic.org/health/treatments/22805-turbinate-reduction).
Can I have turbinate reduction more than once?
Sometimes, depending on your anatomy, symptoms, and what’s causing obstruction now. An ENT evaluation can determine whether swelling, scarring, or other structures are playing the biggest role.
What if I still can’t breathe well after surgery?
Early on, healing-related swelling can temporarily reduce airflow. If problems persist longer-term, an ENT may look for other contributors like septal deviation, nasal valve collapse, polyps, or ongoing rhinitis.
Most “regrowth” concerns trace back to inflammation—especially allergies and irritants—which can be managed.
Conclusion: The Best Way to Keep Results Long-Term
True regrowth is uncommon, but the remaining tissue can swell again—and that swelling is often driven by allergies, irritants, or chronic rhinitis. The best long-term strategy is to treat the cause of inflammation and keep follow-up care on track. If nasal obstruction returns after you initially felt better, an ENT evaluation can clarify whether turbinates are the main issue—or whether something else is contributing.
Ready to get answers tailored to your nose and your triggers? Book an appointment with Sleep and Sinus Centers of Georgia: https://www.sleepandsinuscenters.com/
Disclaimer
This article is for educational purposes only and is not medical advice. Please consult a qualified healthcare provider for diagnosis and treatment.
Don’t let allergies slow you down. Schedule a comprehensive ENT and allergy evaluation at Sleep and Sinus Centers of Georgia. We’re here to find your triggers and guide you toward lasting relief.








